 You will find in this
section hot NEW articles which we feel are of national importance to all folks.
These in-depth scientific forensic works are brought to you as a free service from AAJTS. If you wish to
become a member of the Academy and receive weekly
Articles, join now! You will find in this
section hot NEW articles which we feel are of national importance to all folks.
These in-depth scientific forensic works are brought to you as a free service from AAJTS. If you wish to
become a member of the Academy and receive weekly
Articles, join now!
THE
LIMITED ORTHOPEDIC EXAMINATION WITH ORTHOPEDIC TESTS
The Orthopedic examination has
basic portions:
1.
History
2.
Clinical Examination
3.
Radiographic Imaging and Reading.
HISTORY:
The history is the record of the
patient’s incident whether accidental or unplanned form the day the time
and a step-by-step development until the time of history taking. This
includes any doctors seen, medications taken, changes in pains or any
thing relating to the injury. Generally find out what happened and what
was injured, to whom, where it happened, why it happened, and ho it
happened and the mechanic of the injury or etiological events leading to
the patients condition (In this text I have included various examples of
in-depth questions to ask specifically relative to the type of claim
i.e., Workers Compensation or Industrial, Auto-accident and so forth).
Next ask about pain
correlations. Where is your pain/are your pains? Have
the patient point with their own fingertips to the spot in pain. Ask
the patient to describe the characteristics of the pain such as
“aching”, “burning”, “sharp”, and “dull”. These characteristics tell us
what tissue injuries may be involved.
In cases of workers compensation
or personal injury always have the patient write the history in their
own words after the first visit. Of course you still take a complete
history upon the initial visit. The history in their own words and
writing provides insurance for you in the event of deposition and
discovery, or actual court proceedings.
The next section is past medical
history (Please review actual reports or audits I have included in the
text) any unusual childhood illness. Any past surgeries or tumors
benign or malignant. Any previous industrial or personal injuries.
Ask the following:
·
Age – may determine treatment
·
Present Occupation
·
Previous occupation
·
Hobbies or recreational activities
·
Previous injuries
·
History of any fractures or dislocations.
·
History of any hospitalization for spinal or
extremity injuries.
·
Any past accidents whether industrial or
non-industrial
·
Any allergies
·
Any medications taken and the response
Again, always take the history
in the patient’s own words or at the least as related by the patient.
Taking the patients height,
weight, blood pressure, respiration, and pulse follows the history.
Note the patient’s race, body build (ectomorphic, endomorphic,
mesomorphic, obese) and attitude.
THE BASIC CLINICAL
EXAMINATION
The Clinical examination
consists of three basic sections:
·
Examination of the Part complained of
·
Investigation of possible sources of pain and referred
symptoms
·
General
Examination of the body as a whole
The area of examination must be
exposed with the proper lighting. An Orthopedic inspection is performed
checking the bones for alignment, deformities or shortening. This is
followed by examination of the soft tissues for shape and contours
making sure to make a bilateral comparison. Note any skin
discolorations including cyanosis, pigmentations, etc. Ask and check
for nay signs of scars or sinuses, such as scars from previous
surgeries. Palpate the part complained of checking the bones, skin,
temperature, and soft tissues for signs of spasm, atrophy or wasting any
areas of local tenderness fasciculation’s or an abnormal tissue
consistency. Measurement of the extremities (see examination sheets
provided in this text) for any unusual differences in muscular girth is
commenced. Exact knowledge of atrophied musculature will tell the level
of nerve tissue damage.
Range of motion both active and
passive is initiated with pain responses noted as to degree and
occurrence of pain or manifestations. Note any creptations during the
active and passive motion. In cervicothoracic injuries ROM for the
cervicothoracic spine, shoulder, elbow, wrist and hand is commenced. In
lumbosacral injuries, Lumbosacral rom as well as hip, knee, and ankle
are commenced. Always note the degree of patient pains upon motion as
mild, slight, moderate, and severe and note the motion eliciting the
pain.
Measure the strength and power
of the muscle that are responsible for each movement of the joint. This
is classified into”
0=No contraction (zero)
1=Flicker of contraction (trace)
2=Slight power sufficient to
move the joint (poor)
3=Power sufficient to move the
joint against gravity (fair)
4=Power to move the joint
against gravity plus added resistance (good)
5=Normal power full range of
motion vs. gravity with full resistance. Investigation of any possible
courses of referred symptoms is noted. For example, a patient has
shoulder pain. Investigate the brachial plexus. A pain in the lower
portion of the scapula could indicate a possible gall bladder disease
especially on the right side. This is especially true in susceptible
individuals (Obese female over forty).
Your localization and objective
testing will reveal weakness and its level. You can elicit pain
response with your muscle testing, which can reveal muscle, or joint
(depending on were the pain is located) what is precluding an active
contraction or work activity.
Oftentimes a forensic evaluation
of muscle strength is not considered complete absent a functional
analysis. Thus the patient should be asked to perform maneuvers. For
example arising from a squatted position or stepping onto a chair gives
a good indication of proximal leg strength. Minor’s sign can be noted
if the patient must use their arms on their legs when arising form the
squat. Bouncing while in the Squat position or the “Bounce Home Test”
will indicate the integrity of the feet, ankles, knees, hip joints as
well as the low back. A patient that must push off a chair from a seat
position to arise may have spasm quadriceps weakness. Handgrip strength
or dynamometer testing (test of three). Patients with weakness about
the pelvic girdle may arise from the supine position by first turning
prone, then kneeling and slowly pushing themselves erect by standing
bent forward and using the arms to climb up the thighs (again a +
Minor’s sign).
Examine the spinal cord and
peripheral nerve integrity with spinal level correlation through testing
the deep tendon reflexes. Grade them into classifications:
0=No reflex activity
1=diminished activity
2=normal activity
3=quick activity
4=hyper active
Segmental Level Correlations
Biceps - 2+ Cervical 5, 6
Bra/rad - 2+ Cervical
5, 6
Triceps - 2+ Cervical
7, 8
Knee - 2+ Lumbar
2,3,4
Ankle - 2+ Sacral
1,2
If sensation is disturbed, its
anatomic pattern should be recognized. For example it is well
established that a stocking and glove distribution can be due to
peripheral nerve where a radiating pain or radiculopathy is usually due
to the nerve roots. In any event the finding of motor weakness and
reflex change can determine the anatomic localization of disease or
trauma. This occurs through your synthesis of the data noted and
correlated with your knowledge of the afferent nerves, the synaptic
connections within the spinal cord, and the motor nerves, as well as the
descending motor pathways. Thus much like the EMG, you can determine
much about the integrity of the disc, the motor neuron, the cord and
tissue synaptic connections and the sensory pathway to the cord.
Examine the superficial reflexes
when they correlate with appropriate level of investigation.
Abdominal 2+ Upper
Thoracic 8,9,10
2+
Lower Thoracic 10, 11, 12
Cremasteric 2+
Lumbar 2,3
Plantar
2+ Lumbar 4,5, Sacral 1,2
The following table will aid in
the diagnosis of upper motor neuron lesions from lower motor neuron
lesions through your finding from your reflex testing.
SYSTEMS UMNL
LMNL
DT Reflexes Hyperactive Diminished or absent
Atrophy
Absent Present
Fasciculation’s Absent Present
Tonus Increased Decreased or
absent
It must be noted that
Fasciculation’s (see Nerve Studies) are the most common extraneous
movements seen. They come in the form of brief, fine and irregular
twitches of the muscle visible under the skin. These
Fasciculation’s are indicative
of disease of the lower motor neuron but sometimes can occur in normal
muscle, particularly in the calf muscles of our geriatric populations.
In cervicothoracic or upper
extremities injuries have the patient perform bilateral dynamometer
testing for grip strength. The test is repeated three times by each
hand. Note the injured hand and the handedness of the patient (right
vs. left).
Have the patients walk away from
you and towards you and watch their gait for abnormalities.
Ask them to demonstrate a squat
for you. Note whether they are able to perform the squat or unable to
perform. Note whether the squat was done well.
Ask them to heal walk/and toe
walk for you to determine L5/S1 integrity
(heel walk=dorsiflexion of the toes and ankle which is primarily L5 and
minor L4 and toe walk is the calf muscles primarily the S1 nerve root).
Note whether the patient has
done it well or done poor or not at all. Inability to walk on the toes
indicates alterations in sacral first nerve root integrity as well as
possible lumbar disc fifth involvement. Inability to walk on the heels
indicates lumbar fifth nerve root integrity as well as the lumbar disc
fourth.
Check the patient’s extremity
pulses and check for venous stasis.
Radial
4+/4+
Femoral 4+/4+
Popliteal 4+/4+
Dorsal Pedis 4+/4+
Posterior Tibial 4+/4+
4+ is considered normal for
peripheral bilateral vascular pulses. Note any edema by area and check
for tenderness of the extremity. Check homan’s sign (see orthopedic
tests) bilaterally.
Run the Waltenberg pinwheel down
the dermatome patterns and note whether they are intact or not. Locate
any areas of numbness. Often, a slow and careful assessment of the
dermatomes using a Pin can be more accurate although more time
consuming. It is said, “anything worth doing is worth doing well”.
Segmental Level of peripheral
Nerves.
C2 – Area under the chin
C3 – Area in the front and back
of the neck
C4 – Shoulder area
C6 – Thumb area
C7 – Chiropractic index finger
C8 – Ring and little fingers
T4 – Nipples line
T10 – Umbilical line
L1 – Inguinal area
L3 – Knee area
L5 – Anterior ankle and foot
containing big toe plus two.
S1 – Heal and little toe plus
one.
In cases where you suspect
possible head trauma run a ENT examination checking the ears, eyes, nose
and throat for any possible bleeding (see Neurological Diagnostic
Modalities). Of course check the pupils of the eyes for ipsilateral
dilation, or bilateral dilation or constriction. Check the retina for
any possible hemorrhage or internal cranial edema.
The general examination of the
body as a whole includes a psychological make-up of the patient such as
attitudes, etc. Perhaps the patient only dreamed the incident and their
physical complaint would be better served by a psychologist or
psychiatrist.
Other specific orthopedic tests
would be performed and depending on a cervical spine injury or
lumbosacral injury specific orthopedic test would be correlated with
other special testing.
Radiographic imaging would also
be correlated with the subjective and objective reported thus far.
When you have taken the complete
history, past medical history, review any past medical records and take
a complete physical of areas of complaint, neurological, orthopedic and
x-ray imaging you will be able to correlate all the know objective,
subjectives, ad special tests with the history and conclude the correct
diagnosis and subsequent treatments.
The following are orthopedic
tests utilized for clarification and differential diagnosis of
neuro-musculo-skeletal conditions.
1.
Adson’s
Test
Procedure: With the patient seated,
establish the radial pulse. Have the patient extend their head and
rotate to the side on which the pulse is being taken. Have the patient
take a deep breath and bear down. Extend the arm 45 degrees.
Significance: Radial pulse diminished
or obliterated indicates THORACIC OUTLET SYNDROME.
2.
Brudzinski’s Sign
Procedure: Begin by gently flexing
the patient’s neck onto their chest. If the patient has a moderate
disorder this may feel excruciating. In minimal to slight to moderate
conditions forcibly flex the patient’s neck onto their own chest.
Significance: If the patient’s hips or
legs demonstrate a flexion motion this indicates Meningitis or Disc
Poliomyelitis, meningeal irritation or even subarachnoid hemorrhage.
3.
Compression Tests (a-also known as Cervical Compression Test, b-also
known as Hammer Test)
a. Procedure: With the
patient seated gently press down on the top of their head.
Significance: Pain indicates Intervertebral
Foraminal Encroachment.
b. Procedure: With the
patient seated barely press down on the top of their head with your
little finger.
Significance: Malingering
4. Depression
Test (Also Known as Shoulder Depression Test)
Procedure: Have the seated patient
laterally flex their neck. Depress their shoulder on the opposite side.
Significance: Pain indicates Radicular
Adhesion in the IVF’s.
5.
Distraction
Test (Also known as Cervical Distraction Test)
Procedure: With the patient seated
gently lift cephalad the patient's head to remove its weight from their neck.
Significance: 1. Relief of patient’s
pain indicates Intervertebral Foraminal Encroachment.
2. Pain
indicates spasticity of the cervicothoracic para-
spinal musculature.
6. GSRT
(Global Sustained Rotational Test, named the Neff Test by Rene’ Calliet
in 1982)
Procedure: With the patient seated
or supine take your middle finger and make a contact with the atlas.
Gently rotate the patient’s head and neck to the full range of motion
just entering the manipulative range but not in the interim or through
it. Observe for nystagmus blood shoot eyes that were not there prior to
the test, nausea, dizziness, or vertigo. If negative extend the head
and hold thirty seconds and observe for manifestations
i.e. nystagmus etc.
Significance: Potential for
cervicobasilar infarction or Stroke via interfacial bands and kinks,
bony exostoses with lateralization about the intervertebral artery, and
possible plaque with thrombosis or embolism.
7.
Soto
Hall Test
Procedure: Flex the neck of the
supine patient while pressing gently on the upper sternum.
Significance: Pain indicates Fracture,
Discopathy, Supraspinatous Ligament tear, or dural sleeve adhesions.
8.
Swallowing Test
Procedure: Have the seated patient
swallow.
Significance: If the patient has pain
or difficulty swallowing this indicates a possible Infection,
Osteophytes, Hematoma or tumor in the anterior portion of the cervical
spine.
9.
Valsalva Maneuver
Procedure: Have the patient in a
seated position hold their breath and bear down.
Significance: Pain may indicate a
Discopathy, Spinal Cord Tumor, or any Space Occupying Lesion.
TESTS
SPECIFIC FOR THE SHOULDER AND UPPER ARM
A shoulder
examination must contain four tests; three for dislocation and
instability as well as a soft tissue testing.
10. Drawer
tests – Anterior
Procedure: The shoulder to be tested
is abducted between 80 and 120forward
flexed 0 and 20and
laterally rotated, 0 and 30.
The examiner places one hand on the shoulder and the other on the
relaxed upper arm and draws the humorous forward.
Significance: Movement may be
accompanied by click and/or apprehension.
11. Posterior:
Procedure: Examiner pulls
up on the arm at the wrist while pushing down on the Humerus with the other hand.
Significance: If more than
50% posterior translation @ patient is apprehensive patient has posterior instability.
12. Inferior
Procedure: Also known as
the Sulcus Sign Test. The patient sits with the arm by the side. The
Examiner grasps the patient’s forearm below the elbow and pushes the arm
distally.
Significance: Presence of
Sulcus sign=Inferior
instability.
13.
A/C
Shear
Procedure: Patient seated
examiner cups hands over the deltoid muscle with one hand on the
clavicle and one hand on the spine of the scapula then squeezes the
heels of the hands together.
Significance: Pain or
abnormal movement =
acromioclavicular joint pathology.
14. Speed
Test:
Procedure: Examiner
resists shoulder forward shoulder flexion with the patient's forearm
supinated and the elbow is completely extended.
Significance: Increased
tenderness in the bicipital groove is indicative of bicipital
tendonitis. ST is more effective than Yergason's because ST moves bone
over the tendon during the test.
15. Supraspinatous
Shoulder is abducted 90
with no rotation, and resistance to abduction is provided by the
examiner. The shoulder is then medically rotated and angled
forward 30
so that the patient's thumbs point toward the floor. Resistance to
abduction is again given while the examiner looks for weakness or pain.
Significance: Supraspinatous
muscle or tendon tear,
neuropathy of the suprascapular nerve.
16.
Brachial
Plexus C5-C7 nerve roots
and median nerve-Arm is abducted
and laterally rotated behind the coronal plane with the shoulder girdle
fixed in depression. The elbow is then passively extended with the
wrist held in extension and the forearm in Supination.
Significance: Pain, ache, tingling in the thumb and first three
fingers = median nerve tension or nerve root tension.
17.
Codman's Arm
Drop Patient to fully abduct
arm and lower it slowly.
Significance: If arm
drops to side (patient is unable to lower it slowly) it indicates
ROTATOR CUFF TEAR.
18.
Dugus Test Patient to touch
opposite shoulder with hand. If patient is unable to touch opposite
shoulder, it indicates DISLOCATION.
19. Apprehension
Flex, abduct and externally rotate patient's arm.
Significance: As
external rotation begins to exceed 90
a look of apprehension on the patient's face indicates CHRONIC TENDENCY
TOWARDS DISLOCATION.
20.
Yergason’s Test
Procedure: Gently
flex the patient s elbow 90 degrees. With one hand pull down on the
elbow and stabilize it while moving the patients wrist laterally with
the other hand (to externally rotate the patients arm)
Significance: If the biceps tendon slips out of the bicipital
groove, which at times is palpable, and/or the patient experiences pain
in the region, it indicates a TEAR OF THE TRANSVERS HUMERAL LIGAMENT.
Often time’s pain alone indicates tendonitis of the long head of the
biceps tendon.
TESTS FOR THE ELBOW:
21.
COZEN’S TEST
Procedure: Gently extend and
pronate the arm of the patient and extend their wrist. Stabilize the
elbow and attempt to flex the wrist while the patient resists.
Significance: Excessive motion
indicates a TEAR OF THE COLLATERAL LIGAMENT (Valgus stress = medial
collateral ligament: Varus stress = lateral collateral ligament)
22.
TENNIS
ELBOW TEST – MILL’S MANEUVER
Procedure: With the patient’s
arm pronate, have them flex the wrist. Then have the patient
attempt to supinate the forearm against the
doctor’s resistance.
Significance: Pain at the lateral Epicondyle indicates
LATERAL EPICONDYLITIS. Pain at the
medial Epicondyle indicates MEDICAL
EPICONDYLITIS AKA Golfers Elbow
23.
STABILITY TESTS
Procedure: With the patients
elbow extended, grasp their wrist and distal Humerus. Apply first a
Valgus stress, and then a Varus stress to the elbow.
Significance: Excessive motion indicates a TEAR OF
THE COLLATERAL LIGMENT (Valgus stress=medial
collateral ligament: Varus stress=lateral
collateral
ligament.
24.
TINEL’S ELBOW SIGN
Procedure: Tap ulnar nerve in
groove between olecranon and medial Epicondyle.
Significance: Hypersensitivity indicates NEURITIS,
NEUROMA OR A
REGENERATING NERVE.
TESTS
FOR THE WRIST:
25.
FINKELSTEIN’S TEST
Procedure: Have the patient
make a fist with the thumb tucked inside. Gently force the wrist into
ulnar deviation.
Significance: Pain in the anatomical snuffbox of the
patients hand
indicates STENOSING TENOSYNOVITIS AKA DE QUERVAINS’ DISEASE.
26.
Ligamentous Instability tests.
Procedure: The Patient's arm is stabilized with the examiners
hand on the elbow and the wrist. The elbow is Slightly flexed 30-30.
An adduction or Varus Forces is applied to test the lateral collateral ligament. Then the
examiner places an abduction or Valgus force to test the medial
collateral ligament. Some advocate Varus done with arm in full medial
rotation and Valgus done in full lateral rotation.
Significance: Pain upon stress indicates collateral ligament tear
.
27.
Pronator Teres Syndrome Test
Procedure: Elbow flexed to 90
degrees. Examiner resists pronation as the elbow is extended.
Significance: Tingling or
Paresthesia in median nerve distribution
indicates median nerve
entrapment.
28.
PINCH GRIP
TEST
Procedure: Thumb and first finger should touch tip to tip.
Significance: If pads of
finger and thumb touch then pathology to the anterior interosseous nerve
brach of the median nerve. Thus entrapment of the anterior
interosseous nerve as it passes between the two heads of the Pronator
Teres muscle.
29.
PHALEN’S TEST
Procedure: Flex the wrist of
the patient to the maximum degree possible and hold there for a minute.
Significance: Pain and Paresthesia in the hand
indicates CARPAL
TUNNEL SYNDROME:
30.
TINEL’S
WRIST SIGN
Procedure: Tap the median
nerve of the patient at their flexor Retinaculum.
Significance: Pain and Paresthesia in the wrist and/or
hand
indicates CARPAL TUNNEL SYNDROME.
31.
UNCLES
TEST
Procedure: Extend the wrist of
the patient to the maximum degree possible and hold there for a minute.
Significance: Pain and Paresthesia in the wrist and/or
hand
indicates CARPAL TUNNEL SYNDROME
TESTS FOR
THE HAND
32.
ALLEN’S
TEST
Procedure: Hold the metacarpophalangeal joint of the patient in a few degrees of extension
and try to move the proximal interphalangeal joint into flexion. If
this cannot be done, flex the metacarpophalangeal joint a few degrees aNd
try again to flex the PIP joint.
Significance: Delay in the appearance of the “flush”
indicates PARTIAL OR COMPLETE OBSTRUCTION OF
ONE OF THE ARTERIES.
33.
BUNNEL-LITTLE
TEST
Procedure: Hold the metacarpophalangeal joint of the patient in a few degrees of extension
and try to move the proximal interphalangeal joint into flexion. If
this cannot be done, flex the metacarpophalangeal joint a few degrees
and try again to flex the PIP joint.
Significance: If the
PIP can be flexed in the second position, it indicates TIGHTNESS OF THE
INTRINSIC MUSCLES of the patients HAND. If the PIP cannot be flexed in
either situation it indicates PIP JOINT CAPSULE CONTRACTION.
34.
RETINACULAR TEST
Procedure: Hold the
PIP joint of the patient in a neutral position and try to flex the DIP
joint. If this cannot be done, flex the PIP joint a few degrees and
repeat.
Significance: If the DIP joint can be flexed in the
second position only, it indicates TIGHTNESS OF THE INTRINSIC MUSLES OF
THE HAND OR THE RETINACULAR LIGAMENTS. If the DIP joint cannot be
flexed in either position, it indicates the patient has DIP JOINT
CAPSULE CONTRACTURE.
TEST FOR THE LUMBOACRAL, SACROILIAC,
ILIOFEMORAL JOINTS
35.
LEWIN’S
TEST
Procedure:
Stabilize the supine patient’s thighs upon the table and ask the patient
to sit up.
Significance:
Pain and/or inability to perform may indicate SCIATICA or LUMBAR
ARTHRITIS
36.
MINOR’S
SIGN
Procedure: Observe the patient
rising from the sitting position.
Significance: This may indicate
sciatica if the patient supports Themselves on one side, keeping the
affected side Bent over.
37.
NERI’S
BOWING SIGN
Procedure: The standing
patient is bent forward. Flexion of The knee on the affected side
indicates pain in the leg due to pull on the hamstrings and the pelvis.
Significance: This may indicate sciatica if the
patient supports
themselves on one side, keeping the affected side bent over.
38.
LASEQUE
TEST
Procedure: With the patient in
the supine position, raise their ‘ leg.
Significance: Sciatic pain at
0-30 degrees indicates Altered Sacroiliac joint Dynamics due to a hot
disc assaulting the nerve. Sciatic pain at 30-60 degrees indicates
Altered Lumbosacral Joint Dynamics due to a Sprain.
Sciatic pain at 60-90 degrees indicates Altered L1-L4 joint dynamics.
39.
Well
Leg Raising Test
Procedure: With the same
patient supine, raise the uninvolved leg.
Significance: Sciatic
distribution in the opposite leg Differentiates and demonstrates a
Discopathy.
40.
GOLDTHWAIT
TEST
Procedure: With the patient
supine place on hand under their lumbar spine and raise their leg.
Significance: Pain BEFORE
vertebral motion indicates altered sacroiliac joint Dynamics of SI
Strain/Sprain.
Pain AFTER vertebral movement begins
indicates Altered Lumbosacral or Lumbar joint dynamics of Strain/Sprain.
41.
BECHTEREW’S CHECK TEST
Procedure: Ask your patient to
be seated and extend their legs.
Significance: If the Patient can
extend only one leg at a time, and the ill leg from a Laseque test has
difficulty being Raised this indicates a TRUE SCIATIC CONDITION. If low
back pain occurs during extension, this indicates a possible LUMBAR
DISCOPATHY. If the patient had a positive Laseque test but has no
difficulty sitting ad raiding the ill leg suspect an alleged case of
MALINGERING.
42.
LEG
LOWERING TEST
Procedure: With your patient
in a supine position, flex their thigh 90 degrees and extend their leg.
Ask them to lower their leg and stop half way down.
Significance: If the patient’s leg drops or the patient is unable
to stop, it indicates Discopathy.
43.
GILLET
TEST II
Procedure: With the patient
standing, place one thumb on the 2nd sacral tubercle and
other thumb on the Ilium at the same level. Ask the patient to flex the
thigh.
Significance: If the Ilium fails
to move inferior it indicates a SACROILAC RESTRCTION-STRAIN/SPRAIN.
44.
HIBB’S
TEST
Procedure: With the patient
prone and their knee flexed 90 Degrees internally rotate the femur.
Significance: Increased pain
indicates Altered Sacroiliac joint dynamics due to minimally a strain or
sprain.
45.
FAJERSZTAN TEST-WELL LEG RAISING TEST
Procedure: Perform the
Braggard Test on the Uninvolved Leg.
Significance: Sciatic pain on the
opposite side indicates DISCOPATHY
46.
PATRICK’S FABERE
Procedure: With the patient
supine, place their lateral Malleolus on the opposite knee and depress
the flexed knee.
Significance: Pain in
the Hip indicates OSTEOARTHRITIS OR INFLAMMATION OF THE INVOLVED HIP.
47.
HIBB’S
TEST
Procedure: With the patient
prone, extend and abduct the thigh and push the femur directly into the
Acetabulum.
Significance: Pain indicates
OSTEOARTHRITIS OF THE HIP OR SYNOVITIS.
48.
YEOMAN’S TEST
Procedure: With the patient
prone, extend the thigh and push the femur directly into the Acetabulum.
Significance: Pain indicates OSTEOARTHRITIS OF
THE HIP OR SINOVITES.
49.
ELY’S
TEST
Procedure: With the patient
prone, grasp both ankles and flex the knees upon the thighs.
Significance: If the patient reports pain in the lumbar or
lumbosacral area indicates ALTERED LUMBAR OR
LUMBOCARL JOINT DYNAMICS
due to spastic internal and external rotator of the leg.
50.
GAENSLEN’S TEST-SI SPECIFIC TEST
Procedure: With the patient
supine, flex on thigh onto the abdomen and hold it there. Next,
hyperextend the other hip by slowly lowering the femur ff the table.
Gently apply downward pressure on the hyperextended thigh.
Significance: Pain indicates
ALTERED SCROIIAC JOINT DYNAMICS AND SPRAIN.
51.
MILGRAM’S TEST
Procedure: Have the supine
patient raise their extended legs two inches and hold for 30 seconds.
Significance: Pain or inability
to hold position indicates
INCREASED INTRATHECAL PRESSURE AND/OR DISCOPATHY.
52.
NAFFZIGER’S
TEST
Procedure: With the patient in
the supine posture, compress the jugular veins for 30 seconds and then
ask the patient to cough.
Significance: Pain indicates INCREASED INTRATHECAL PRESSURE AND/OR
DISCOPATHY, DISCOGENIC DIESEASE.
53.
KERNIG’S TEST
Procedure: With the patient
supine, flex their thing on their hip 90 degrees with the knee flexed 90
degree. Ask the patient to extend their knee.
Significance: Inability to extend the knee past 135 degrees
indicates MENIGEAL IRRITATION OR MENINGITIS AND POLIOMYELITIS.
54.
BURN’S BENCH
TEST
Procedure: Have the patient
kneel on a bench. Grasp the ankles and ask the patient to touch the
floor.
Significance: A claim that pain
prevents this motion indicates MALINGERING.
55.
FFEN
TEST
Procedure: Palpate a given
area and ask the patient if this is painful. Come back to it later and
run a pin wheel down the dermatome over the area and ask the patient
what they can feel or are they numb?
Significance: Coached patients
know they have pains ad have numbness. Oftentimes if the patient is
not truly experiencing the problem they get confused and forget what
part is numb and which part is painful. However it is not consistent
for a patient to have severe palpable muscular pain and numbness of
the same tissues at the same time.
TESTS FOR THE HIP AND
PELVIC JOINTS
56.
LEG
LENGTHDISCRPANTY-TRUE LEG LENGTH
Procedure: Measure from the patients ASIS to their medial
malleolus. If discrepancy in length exists, flex hip and knees.
Observe whether the knee of one leg is higher or more anterior than the
other.
Significance: One knee HIGHER
indicates discrepancy in TIBIA LENGTH. One knee ANTERIOR indicates
discrepancy in FEMUR LENGTH.
57.
LEG
LENGTH DISCREPANY – APPARENTY LEG LENGTH
Procedure: Measure from the
umbilicus to the medial malleolus.
Significance: If this differs from leg to leg, and ASIS to
malleolus measurements are equal, the discrepancy indicates PELVIC
OBLIQUITY.
58.
DEARFILED TEST
Procedure: With the patient in
the prone position, check their leg length at the medial malleoli. If
discrepancy exists, flex their knees and gently stretch by Dorsiflexion the feet and recheck.
Have the patient turn their head to the side and recheck.
Significance: If the short leg
becomes the long leg on knee flexion, it indicates an ALTERED SACROILIAC
JOINT. If turning the head alters the leg length, it indicates ALTERED
CERVICAL JOINT DYNAMICS.
59.
OBER’S
TEST
Procedure: With the patient on
their side, abduct and extend their thigh and then drop it.
Significance: If their leg fails to descend or descends in clonic
anner, it indicates CONTRACTURE OF THE TENSOR FASCIA LATA TISSIE.
60.
THOMAS TEST
Procedure: With the patient
supine, flex one knee onto their abdomen.
Significance: Involuntary flexion
of the opposite hip indicates HIP JOINT FLEXION CONTRACTURE.
61.
TRENDELENBERG SIGN
Procedure: With the physicians
hands on the patient’s iliac rests, have the standing patient flex on
hip.
Significance: If their hip on the flexed side fails to raise, or
if it falls, this indicates a WEAKNESS OF THE OPPOSIE GLUTEUS MEDIUS OR
SACROILIAC JOINT SPRAIN.
62.
ANVIL
TEST
Procedure: With the patient in
the supine position, tap their inferior Calcaneus.
Significance: Pain indicates FEMORAL FRACTURE:
TEST
FOR THE KNEE
63.
GRINDING TEST FOR THE PATELLA
Procedure: With the patient
supine, push the patella distally. Ask the patient to contract the
quadriceps against resistance to the patella’s upward movement.
Significance: Palpable crepitus
as the patella moves upward indicates ROUGHENING OF THE ARTICULAR
SURFACE.
64.
REDUCTION CLICK TEST
Procedure: With the patient
supine, flex their knee while rotating it both internally and
externally. Then extend the knee while continuing to rotate it.
Significance: A clicking sound
during extension and rotation indicates that the damaged MENISCUS HAS
SLIPPED BACK INTO PLACE.
65.
EFFUSION TEST-MAJOR
Procedure: With the patient
supine, push the patella down into the Trochlear groove and quickly
release it.
Significance: If the patella rebounds (a blottable patella) this
indicates JOINT EFFUSION.
66.
EFFUSION
TEST-MINOR
Procedure: With the patient supine, push the patella
from the Suprapatelar pouch to the infrapatelar area den then from
lateral to medial. Next tap the medial side of the knee just posterior
to the patella.
Significance: If a fluid wave
causes fullness on the lateral side of the joint, it indicates MINOR
EFFUSION.
67.
APPRENHENSION TEST
Procedure: With the patient supine, push their patella
laterally.
Significance: A look of apprehension on the patient’s face
indicates a CHRONIC TENDENCY TOWARDS FREQUENT LATERAL DISLOCATION.
68.
TINEL’S KNEE SIGN
Procedure: Tap the infrapatelar branch of the saphenous nerve
at the medial side of the Tibial tubercle.
Significance: Hypersensitivity
indicates NEURITIS, NEUROMA OR A REGENERATING NERVE.
69.
DRAWER SIGN
Procedure: With the patient’s knee flexed and foot stabilized
Flat upon the table, move the patient’s proximal Tibia anterior and
posterior.
Significance: Abnormal anterior movement indicates RUPTURE OF THE
ANTERIOR CRUCIATE LIGAMENT. abnormal posterior movement indicates
RUPTURE OF THE POSTERIOR CRUCIATE LIGAMENT.
70.
APLEY’S COMPRESSION TEST
Procedure: With the patient prone and their knee flexed 90
degrees, stabilize the leg and place direct pressure firmly on the heel
directed through the tibia. As the menisci are compressed between the
tibia and femur, rotate the leg internally and externally.
Significance: Pain on the medial side of the knee indicates MEDIAL MINISCUS DAMAGE. Pain on the lateral side of the knee is indicative of
LATERAL MENISCUS DAMAGE.
71.
APLEY’S DISTRACTION TEST
Procedure:
With the patient in the same positioin as for the compression test,
traction the patients leg upwards while at the same time gently rotating
it internally and externally.
Significance: Pain
indicates COLLATERAL LIGAMENT DAMAGE
72.
McMURRAY’S TEST
Procedure: With the patient supine, fully flex and externally
Rotate their leg, while maintaining the rotation, Slowly extend the leg
while palpating the joint space and applying posterior force to the
knee. Repeat with internal rotation.
Significance: A painful click on extension with EXTERNAL ROTATION
indicates MEDIAL MENISCUS TEAR, with INTERNAL ROTATION, LATERAL MENISCUS
TEAR.
73.
STABILITY KNEE TEST
Procedure: With the patient seated, slightly flex their knee
and push laterally on the ankle and medially on their knee (Valgus
stress). Repeat while pushing medially on the ankle and laterally on
the knee (Varus stress).
Significance: Palpable gapping on the medial side of the knee
under VALGUS STRESS indicates MEDIAL COLLATERAL LIGAMENT TEAR. Gapping
on the lateral side of the knee under VARUS STRESS indicates LATERAL
OLLATERAL LIGAMENT TEAR.
TESTS
FOR THE ANKLE AND FOOT
74.
DORSIFLEXION TEST
Procedure: With the patient seated extend the leg and try to dorsiflex their ankle. If Dorsiflexion is limited, flex their knee and
repeat.
Significance: Limitation of motion in both positions indicates SOLEUS MUSLCE TIGHNESS. LOM on knee extension only indicates
GASTROCNEMIUS TIGHTNESS.
75.
ACHILLES CONTINUITY TEST
Procedure: Squeeze the patient’s calf muscles posterior to
anterior.
Significance: Lack of slight
plantar flexion indicates ACHILLES TENDON RUPTURE.
76.
STABILITY TESTS-DRAWER SIGN
Procedure: With the patient’s
foot hanging free, pull their Calcaneus forward while pushing their
distal tibia posteriorly.
Significance: Abnormal forward
motion indicates ANTERIOR TALOFIBULAR LIGAMENT TEAR.
77.
STABILITY TESTS-LATERAL SIGN
Procedure: Passively invert the patients Calcaneus.
Significance: Gapping and rocking of the Talus indicates TEAR of
the ANTERIOR TALOFIBULAR and/or CALCANEOFIBULAR LIGAMENT.
78.
HOMAN’S SIGN
Procedure: With the patient supine dorsiflex the patient’s
ankle.
Significance: Calf tenderness indicates deep vein
THROMBOPHLEBITIS.
79.
BOUNCE HOME TEST
Procedure: With the patient supine, flex the knee. Holding
their ankle passively extend their knee.
Significance:
If the patient's knee fails to fully extend and offers a rubbery
resistance to further extension and ending in a sharp end point this
indicates MENISCUS DAMAGE.
80.
TOE-HEAL WALKING TEST
Procedure: Have
the patient first walk on his heals and then on his toes.
Significance:
An inability to walk on the toes indicates a first sacral nerve root
involvement (5th Lumbar Disc). Whereas an inability to walk on
the heels is indicative of a 5th lumbar nerve root involvement (4th
lumbar disc).
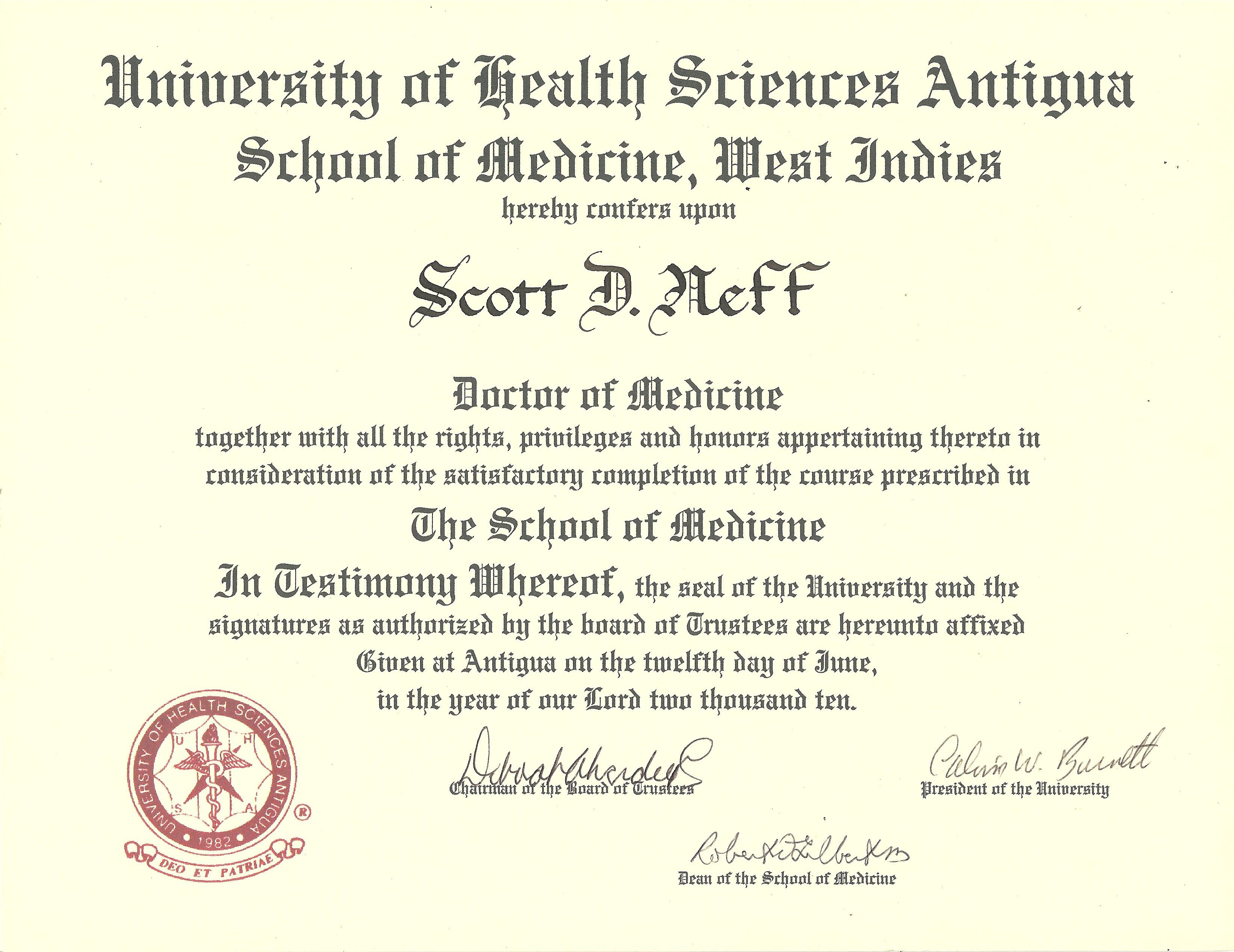
by
Dr. Scott D. Neff, DC
DABCO MPS-BT
CFE DABFE FFABS FFAAJTS, 2010 Graduate Antigua
School of Medicine, West indies made for the medical students of our
times and as a dedication to the
people of America and our world.
©
"Why does this magnificent applied
science which saves work and makes life
easier, bring us little happiness? The simple answer runs, because we
have not yet learned to make sensible use of it." Albert Einstein 1931
GET MORE
ARTICLES LIKE THIS! |
![]()