 You will find in this
section hot NEW articles which we feel are of national importance to all folks.
These in-depth scientific forensic works are brought to you as a free service from AAJTS. If you wish to
become a member of the Academy and receive weekly
Articles, join now! You will find in this
section hot NEW articles which we feel are of national importance to all folks.
These in-depth scientific forensic works are brought to you as a free service from AAJTS. If you wish to
become a member of the Academy and receive weekly
Articles, join now!
THE LIMITED CLINICAL
NEUROLOGICAL EXAMINATION
The Neurological portion of your
examination would include testing the musculature associated with the
nerve level in question. Further, the tests your reviewed in
Orthopedics would be coordinated to determine nerve level integrity.
Thus whenever you examine the spine or extremities you coordinate your
Orthopedic examination with your neurological examination including the
deep tendon reflexes, sensation testing when appropriate for the nerve
level relative to your specific Kinesiological weakness testing for
specific nerve levels.
DIFFERENTIAL DIAGNOSIS
BEFORE THE EXAM BEGINS THROUGH ATYPICAL GAITS
When the patient first enters your office, observe for atypical gaits.
Of course, you can add your gait analysis any time the patient
ambulates.
1.
When an inverted foot is noted upon walking,
examine the lateral leg compartment.
2.
When the patient is noted as walking on their
heels, examine their posterior leg compartment.
3.
When the patient is noted as dragging their
toes, examine the anterior leg compartments.
4.
Look for the Waddling gait of Pagets or
Duchennes Muscular Dystrophy.
5.
Toe Walking Gait of Muscular Dystrophy.
DEEP TENDON REFLEXES:
In your review of the orthopedic section, we detailed deep tendon reflex
testing. Here we will delve deeper into the exact mechanism for such
tests.
CERVICAL SPINE AND UPPER
EXTREMITIES:
Of course, there are three basic deep
tendon reflexes, which evaluate the integrity of the C5, C6 and C7 nerve
supply. These are known as the biceps reflex, the Brachioradialis
reflex, and the triceps reflex. Deep tendon reflexes are of course
considered a lower motor reflex. Here the signal translates to the
posterior horn of the spinal cord, thought internuncial neurons into the
anterior horn cells and returning through the peripheral nerves to the
musculature.
BICEPS REFLEX Ė C5
Although there are multiple innervations to the biceps via C5 and C6,
primary innervation is associated with C5.
Ask the patient to place their arm over you contralateral forearm.
With his arm relaxed, tap your thumbnail with the arrow end of the
reflex hammer. The biceps will jerk slightly for a normal response. If
you attempt the test a few times and no response is elicited perhaps
there is a lower motor neuron lesion somewhere between the C5 nerve
level and the innervation of the biceps muscles. However if the
elicited response is excessive it may be associated with an upper motor
neuron lesion. An example of an upper motor neuron lesion would be cervico-basilar infarction or stoke. An example of a lower motor neuron
lesion may be disc herniation with subsequent peripheral nerve
irritation. Record reflexes as 2 plus for normal, 3 plus or 4 plus for
increased or 0 to 1 plus for decreased reflexes. The opposite extremity
reflex and coordinate date.
BRACHIORADIALIS REFLEX Ė C6
Although there are multiple innervations to the Brachioradialis via
C5 and C6, primary innervation is associated with C6.
Your doctor patient position is the same as with the C5 test. With
the flat edge of the reflex hammer, tap the brachio-radialis tendon at
the distal end of the radius to elicit a radial response. Test the
opposite arm ad compare and record the date.
TRICEPS REFLEX Ė C7
The triceps muscle is innervated by the
radial nerve primarily C7.
The doctor patient position is similar to the previous test save
the fact that you elevate your stabilizing arm slightly. When the
patient is relaxed, tap the triceps tendon where it crosses the
olecranon fossa with the arrow end of the reflex hammer. Compare
bilaterally and record data.
LUMBOSACRAL SPINE AND LOWER EXTREMITIES:
PATELLAR REFLEX Ė L2, 3, AND 4
Although the patella
reflex, or knee jerk, is a deep tendon reflex, innervated by L2, L4 and
L4 primary innervation comes from L4.
Ask the patient to sit on the edge of the examining table with
their legs dangling free. Palpate the soft tissue depression on either
side of the infrapatelar tendon. Tap the tendon with the arrow end of
the reflex hammer, with a short, wrist action. If the test is difficult
to elicit, ask the patient to grasp his their hands together and attempt
to pull them apart as you attempt the test. Compare bilaterally and
records the date.
ACHILLES TENDON REFLEX Ė S1
The S1 nerve level innervates the Achilles tendon deep reflex.
Ask the patient to sit on the edge of the examining table with
their legs dangling. Gently dorsiflex the foot. Tap the tendon with
the flat end of the reflex hammer. If the test is difficult to elicit,
as the patient to grasp their hands together and attempt to pull them
apart as you attempt the test. Compare bilaterally and record the data
for later synthesis.
COMPLETE LIST OF THE DEEP
TENDON REFLEXES
1.
Maxillary reflex aka Jaw Jerk innervation
Cranial Nerve V3. When there is a sudden closure of the jaw when you
strike the middle of the chin, as the mouth was initially open.
2.
Bicep reflex C5 primarily (C6)
3.
Triceps reflex C6 primarily (C7)
4.
Periosteoradial C7 primarily (C6, C8)
5.
Periosteo-Ulnar reflex C8, T1. There is
extension and ulnar abduction of the wrist when the styloid process of
the ulna is struck.
6.
Wrist Reflexes C7, C8. There is flexion or
extension motion when the corresponding tendons are struck.
7.
Patellar reflex L4, (L2, L3). There is
extension at the knee when the patellar tendon is struck. Absence of the
reflex is known as WESTPHALíS SIGN. When the reflex cannot be obtained
and you have the patient clasp their hands together, clench, and the
reflex is obtained you have utilized the JENDRASSIK method of
reinforcement.
8.
Achilles reflex S1, S2.
NERVE LEVEL & PERIPHERAL
NERVE SENSATION TESTING AND VERIFICATION
Sensory testing for the cervical spine is associated with the integrity
of the dermatomes. Dermatomes into the upper extremities include levels
C5 to T1. The following is an outline the brachial plexus distribution
of the upper extremities.
C5 Ė Lateral arm Ė Axillary nerve
C6 Ė Lateral forearm, thumb, index, and half of middle finger Ė sensory
Branches of the Musculo-Cutaneous nerve.
C7 Ė Middle finger
C8 Ė Ring and little fingers, medial forearm Ė medial antebrachial-cutaneous
nerve.
T1 Ė Medial arm Ė medial brachial cutaneous nerve.
While performing the tests, it is expedient to utilize the Waltenberg
pinwheel. If the patient states that they feel the wheel with no
abnormal sensation write intact. If there is numbness write not intact.
The following is a chart of the root to be tested, muscles associated as
well as area of sensation.
ROOT
DISC REFLEX MUSCLES SENSE
C5 C4-C5 Biceps Deltoid Lateral
Arm
Biceps Axillary nerve
C6
C5-C6 Brachio- Biceps Lateral Forearm
Radialis Wrist Extensors
Musculo
cutaneous
C7 C6-C7 Triceps Triceps
Middle finger
Finger
Extensors Wrist Flexors
C8 C8-T1 Finger flexors
Medial Forearm Intrinsic
muscles Me. Ant. Brach.
Of the
hand Cutaneous nerve.
T1 T1-T2 Intrinsic
muscles Medial Arm
Of the
hand Med. Brach.
Cutaneous Nerve.
Next, test the peripheral nerves. Utilize the following chart for
evaluation of the peripheral nerves.
NERVE
MOTOR TEST SENSATION
Axillary Deltoid Lateral Arm
Ė Deltoid patch on
Upper arm
Musculo-Cutaneous Biceps Lateral Forearm
Radial Wrist Extension Dorsal web space
between Thumb and index finger
Median Thumb Pinch Distal radial
aspect Ė index
Finger
Ulnar Abduction Ė little Distal ulnar
aspect Ė little finger
SENSATION TESTING FOR THE LUMBAR SPINE
Testing of the dermatomes of the lower extremity serves to indicate
nerve level of the lumbosacral spine. The following chart will
coordinate nerve level with reflex, musculature and area of sensation.
ROOT
DISC REFLEX MUSCLES SENSATION
L4 L3-L4 Patellar Anterior
Medial leg and Tibialis Foot
L5 L4-L5 None Extensor
Lateral leg & Hallucis
longus dorsum of foot
S1 L5-S1 Achilles Peroneus Longus Lateral
Foot and Brevis
THE SUPERFICIAL REFLEXES
The superficial reflexes (i.e. abdominal, cremasteric, and anal
reflexes) or upper motor neuron reflex testing is mandatory when we
suspect specific lesion associated with an upper motor neuron lesion.
The absence of the superficial reflex perhaps indicates an upper motor
neuron lesion. If the superficial reflex is absent and the deep tendon
reflex is increased, this will add evidence to indicate an upper motor
neuron lesion and reason for consultation for Neurodiagnostic testing.
ABDOMINAL REFLEX
The patient is asked to lie in the supine position. Place
the arrow end of the reflex hammer upon the abdomen and stroke each
section of the abdomen, noting whether the umbilicus moves toward the
area being stroked. The lack of an abdominal reflex may indicate
an upper motor neuron lesion provided you perform the test correctly.
You may also detect a lower motor neuron lesion because the upper
muscles of the abdomen are innervated form T7 through T10. The
lower muscles from T10 to L1. Thus, lack of a reflex will indicate
the approximate level of a lower motor neuron lesion.
CREMASTERIC REFLEX
The patient is asked to lie in the supine position. Stroke the
inner aspect of the upper thigh with the arrow end of the reflex
hammer. If the reflex is elicited the scrotum will be pulled upward as
the cremasteric muscle contracts. This is associated with a T12 level.
If the reflex is reduced or absent bilaterally this may indicate an
upper motor neuro lesion, while a unilateral absence indicates a
probable lower motor neuro lesion between L1 and L5.
ANAL REFLEX
The patient is asked to lie in the prone position. Gently touch
the perianal skin. The external and anal sphincter muscles (S2, S3, S4)
would contract in response.
ANAL WINK REFLEX
If you are unable to elicit a response, take a finger cot, place
your finger gently within the anus, and pull out. The anus should
contract as if to wink.
CLINICAL UNDERSTANDING OF UPPER AND
LOWER MOTOR NEURON LESIONS
Before a complete review of the pathological reflexes to determine upper
and lower motor neuron lesions, a complete understanding of these signs
and symptoms will make the diagnosis of the pathological reflex via
common scientific sense.
The motor innervation of the striated musculature is innervated by the
Pyramidal system. The Pyramidal pathway conducts impulses to the
spinal cord anterior horn cells associated with isolated movements of
the hands ad fingers which form the basis for the development of manual
skills. In fact, it has been estimated that 55% of all pyramidal
fibers end in the cervical cord, 20% in the thoracic and 25% in the
lumbosacral segments. Therefore, the muscles of the upper
extremity are more affected than the muscles of the lower extremity and
the distal muscles (hand) are most affected compared to the proximal
because they have more motor units for complex actions.
UPPER MOTOR NEURON LESION AKA
SPASTIC PARALYSIS AKA SUPRANUCLEAR PARALYSIS
1.
Initially there is loss of tone in the
affected muscles (hypertonia)
2.
Soon after the muscles gradually become
resistant to passive movement and yield SPASTIC PARALYSIS.
3.
The myotatic deep tendon reflexes, especially
in the leg, are increased in force and amplitude known as HYPERREFLEXIA.
4.
The SUPERFICIAL REFLEXES are lost or
diminished.
5.
Positive Babinskiís Sign is noted.
6.
If the suspected lesion is above the pyramidal
decussation, the symptoms will be found on the contralateral side.
7.
If the suspected lesion is below the pyramidal
decussation, the symptoms will be found on the ipsilateral side.
With an upper motor neuron lesion the first manifestation will be a
disturbance in muscular tonus, expressed as hypotonia. However, within
2-3 weeks changes occur leading to hypertonia bringing about
hyperreflexia. Thus when hyperreflexia is noted the lesion must be
considered at least 2-3 weeks old.
The reason that UMNLís lead to a loss of the superficial reflexes
is due to the fact that there is retrograde degeneration. This
retrograde degeneration causes degeneration of the association neuron
and the afferent sensory neuron in the reflex arc.
In the geriatric population, there is a tendency for the
superficial abdominal reflexes to be absent. Thus, this may not
indicate an UMNL.
It must also be noted that absence of the superficial abdominal
reflexes is not in itself indicated of a MNL. Finally, in UMNLís
flaccidity and atrophy will be greater in the upper extremities in the
distal aspect because there are more motor units present.
LOWER MOTOR NEURON LESION AKA FLACCID
PARALYSIS LESION
1.
Muscle fibers, which have been deprived of
their afferent nerve innervation, become completely paralyzed.
2.
All reflexes, deep tendon and superficial are
abolished and the musculature become flaccid.
3.
The muscle fibers begin to undergo progressive
atrophy.
4.
There are marked fibrillary tremors and
fasciculations noted in the affected musculature within three weeks of
the initial injury.
5.
Lower motor neuron lesions produce ipsilateral
symptoms except for the Ivth cranial nerve because the IV crosses.
It must be noted that when the lesion is found in the anterior r
horn cells, it will take two weeks or more for paralysis and flaccidity
to occur. Generally, marked fasciculations and fibulation occurs while
the LMN is degenerating then they disappear. If the fasciculations
occur months to years later, it indicates that there is some nerve
regeneration. When this is noted you will have excellent results
PATHOLOGICAL REFLEXES COMPLETE BY BODY
REGION
Pathological reflexes act reciprocally to the previous. The
presence of a pathological reflex may indicate an upper motor neuron
lesion and its absence indicates the norm.
HEAD
1.
BABINSKIíS PLATYSMA SIGN
If resistance to flexion of the chin against the chest is presented or
opening the mouth, the platysma on the side will contract, whereas the
affected side will not.
2.
HEAD RETRACTION REFLEX
Specific downward percussion upon the upper lip with the patientís head
slightly in forward flexion produces head and neck bending followed by
brisk head retraction.
3.
Mc MCCARTHYíS SIGN AKA The Glabella Reflex
With the patient in the supine position gently percuss the Supraorbital
ridge which results in the reflex contraction of the Obicularis Oculi
muscle.
4.
SNOUT REFLEX
Specific tapping of the middle of the upper lip induces an exaggerated
reflex contraction of the lips.
UPPER EXTREMITIES
1.
BABINSKIíS PRONATION SIGN
The patient is in the sitting position. Ask the patient to place their
hands in approximation with the palms upward. Place your fists below
the patient hand. Bring your fists upward jarring the patientís hands
several times. The affected hand will fall in PRONATION, and the sound
hand will remain horizontal.
2.
BECTEREWíS SIGN
The patient is in the sitting position. Ask the patient to flex and
relax the forearms several times. The paralyzed forearm will fall back
slowly and in a jerky manner, even when contractures are mild.
3.
CHADDOCKíS WRIST SIGN
Gently stroke the ulnar side of the forearm near the wrist. Flexion of
the wrist, and extension and fanning of the fingers will indicate the
affected hand.
4.
TROMNERíS SIGNS AKA Finger Flexion Reflex
A positive sign is elicited by specifically tapping the palmar surface
or the tips of the middle three fingers produces prompt flexion of the
fingers.
5.
GORDONíS FINGER SIGN
Extension of the flexed fingers or the thumb and index finger when
pressure is exerted over the Pisiform bone.
6.
HOFFMANíS SIGN
This sign is demonstrated by a clawing movement of the fingers produced
by the flicking of the distal phalanx of the index finger. The thumb is
also clawed.
7.
FORCED GRASPING TEST
Specifically stroke radial ward with your fingers across the patientís
palm causes a grasp reaction of the hand.
8.
KLEISTíS HOOKING SIGN
Exert pressure with your hand against the patientís flexor surface of
the fingertips. A sudden reactive flexion of the fingers indicates the
affected hand.
9.
KLIPPEL AND WEIL THUMB SIGN
Ask the patient to flex their fingers. Quickly extend the patients
fingers with your hand. A positive test is demonstrated by flexion and
abduction of the patientís thumb.
10.
LERIíS SIGN
Absence of normal flexion of the elbow upon forceful passive flexion of
the wrist and fingers.
11.
MAYERíS SIGN
Ask the patient to supinate their hand. Absence of adduction and
opposition of the thumb upon passive forceful flexion of the proximal
phalanges, especially of the third and fourth fingers, of the supinated
hand.
12.
SOUQUEíS SIGN
In attempting to raise the paralyzed arm, the fingers spread out and
remain separated.
13.
STRUMPELLíS PRONATION SIGN
Upon the patient flexing the forearm, the dorsum of the hand approaches
the shoulder instead of the palm.
LOWER EXTREMITIES
1.
ANKLE CLONUS
The patient is seated or supine. Place your stabilizing hand upper the
patient popliteal space. Forcibly and quickly dorsiflex the patientís
foot. A positive test demonstrates and continued rapid flexion and
extension of the foot. A rapidly exhaustible clonus may be normal.
2.
BABINSKIíS SIGN
With the metal end of the reflex hammer, stimulate the plantar
surface
of the foot from the Calcaneus along the lateral aspect to the
forefoot. Seeing the big toe extend while the other toes plantar flex
recognizes a positive test. This would indicate an upper motor neuron
lesion indicating brain pathology or trauma. In the newborn, a positive
test is normal. Shapiro advices forcible flexing of the second to fifth
toes while eliciting the Babinskiís response in the usual manner, for a
more definitive test.
3.
CHADDOCKíS SIGN
Babinski response obtained by the stroking of the lateral malleolus.
4.
CROSSES EXTENSION REFLEX
Ask the patient to lie supine on the examining table. Have the patient
flex both legs. Stimulate the sole of the foot, which causes extension
of the contralateral leg.
5.
EXTENSOR THRUST
Extension of a flexed lowed limb when the sole of the foot is forced
upward.
6.
GONDA REFLEX
Press one of the patientís toes downward and release it with a snap.
The reflex is an upward movement of the Big Toe.
7.
GORDONíS LEG SIGN
Squeezing the patientís calf will elicit a Babinski like response.
8.
GASSET AND GAUSSEL SIGN
Ask the patient to lie in the supine position. The patient will be able
to raise either leg separately but cannot raise both legs
simultaneously. If the paralyzed leg is raised, it will fall back
heavily when the examiner raises the unaffected leg.
9.
HIRSCHBERGíS SIGN
Stroke the inner border of the foot. The reflex will cause adduction
and internal rotation of the foot.
10.
HOOVERíS SIGN
With the alleged Hemiplegic patient in the recumbent position, place the
palms of your hands directly beneath the patientís heels, while the
patient is asked to pres down Pressure should be felt only from the heel
of the non-paralyzed leg. Next remove our hand from beneath the
non-paralyzed heel and place it o the dorsum of their foot, and the
patient is instructed to raise the healthy leg against this resistance.
If the patient has a true organic HEMIPLEGIA, the hand remaining beneath
the heel of the paralyzed leg will feel no added pressure. However, if
the patient has a hysterical paralysis, the heel of the supposedly
paralyzed leg will press down against the examinerís had as an attempt
is made to raise the healthy leg.
11.
HUNTINGTONíS SIGN
Flexion at the hip, extension at the knee, and elevation of the affected
weak lower extremity upon coughing and straining.
12.
MARIE AND FOIX RETRACTION SIGN
Upon the forcing of the patientís toes downward, the knee and hip are
drawn into flexion (important
test).
13.
MANDEL-BECHTEREW SIGN
Flexor movement of the four outer toes upon striking the dorsum of the
foot over the cuboid bone.
14.
NERIíS SIGN
The patient is in the recumbent position. Ask the patient to
alternately raise one leg at a time. The knee of the paralyzed side
flexes, the other remaining straight. Forward flexion of the trunk in
the standing position causes the paretic lower lib to flex while the
normal one remains straight.
15.
OPPENHEIMíS SIGN
Run the metal handle end of the reflex hammer along the crest of the
tibia and the Tibialis anterior muscle. A normal test indicates no
reaction or the patient complains of pain. A positive test extends the
great toe while the other toes plantar flex.
16.
PATELLAR CLONUS AKA TREPIDATION SIGN
Forcibly depress the patella with a quick movement while the leg is in
extension and relaxed. A positive reflex is a rapid up and down
movement.
KINESIOLOGY-PERIPHERAL NERVE INTEGRITY
TESTING CORRELATED WITH MUSCULAR POWER
Kinesiology is defined as that branch of biomechanics, which studies the
science of movement. In general, it is divided into two fields of
study.
1.
Osteokinematics, which is that branch of
Kinesiology, which attempts to focus primarily on overall movement of
bones, with little reference to their related joints.
2.
Arthrokinematic, which is that branch of
Kinesiology, which attempt to focus on the intimate and delicate
mechanics of joints.
Early you studied Kinesiology related to a motion exam testing the
spine and determining the end feel of the joint and its subsequent
status. Know you will review the testing of the human muscle as a
source for information about motor power, sensation, and segmental level
of peripheral nerve involvement. Any pathomechanical disorder affecting
the cord and nerve roots specifically will produce manifestations in the
extremities reflexive of the vertebral levels involved. As stated and
demonstrated in the Orthopedic Chapter, knowledgeable documentation and
coordination of information about segmental level of peripheral nerve
involvement comes in the form of noting intact dermatomes and reflexes.
Although these are also contained in a neurological examination, they
are not exclusive to a neurological examination. However, when we
measure for atrophy, we were beginning to shift our orientation towards
the neurological interpretation. There we determined neurological level
of involvement by understanding which nerve levels innervated the upper
extremities vs. lower extremities and which level related to specific
muscles. Thus a muscle, which was atrophied, would give us a clue to a
level of disc protrusion or irritation of nerve roots.
Obviously, it is known that pressure on nerve roots causes
diminishing muscle strength. In the Scientific Kinesiological
examination you will be testing for this muscular weakness and
coordinate the data to spinal level and neurological level of origin.
In the neurological portion of the examination always try to coordinate
the motor, deep tendon reflex, and dermatome sensation.
MUSCLE TESTING
Muscle testing is an art and science. Because of all the fraud
associated with Muscle testing (i.e. magnet, vitamin, etc fraud), this
science is best studied by physicians from a nerve level point of view.
Muscle test for nerve levels cervical fifth through the thoracic spine
will follow. In evaluating the cervicals, muscle testing of the
shoulder has demonstrated excellent clinical data. When muscle testing
for cervical integrity the shoulder must be brought through nine
motions: Flexion, extension, abduction adduction, external rotation,
internal rotation, scapular elevation (shoulder shrug), scapular
retraction (position of attention), and shoulder protraction
(reaching). Testing will be classified according to joint motion and
coordinated with the other objective findings.
Always note muscle power data with the 0-5 scales as follows:
0=Non Contraction (Zero)
1=Flicker of contraction (Trace)
2=Sight power sufficient to move the joint (poor)
3=Power sufficient to move the joint against gravity (fair)
4=Power to move the joint against gravity plus added resistance (good)
5=Normal power with a full range of motion against gravity with full resistance.
KINESIOLOGICAL EXAMINATION OF THE
CERVICAL SPINE MUSCULATURE:
In the cervical spine examination, have the patient seated.
You will begin by testing the intrinsic muscle in the neck and cervical
spine as that may restrict motion when spastic and motor weakness, which
can restrict or enhance cervical motion occur.
FLEXION
Flexion of the cervical spine is primarily accomplished by the sternocleidomastoidius muscles acting bilaterally and innervated by the
spinal accessory, or cranial XI nerve.
Stand in front of you patient. Place your left hand upon the patientís
sternal area. Place your right resistance hand upon the patientís
forehead with a broad palmer contact. Ask the patient to forward flex
his neck slowly, while you gradually increase the resistance until you
determine patient overcome resistance.
EXTENSION
Extension of the cervical spine is primarily accomplished by the
cervical paraspinal extensor (capitis, semispinalis, Splenius etc) and
the Trapezius innervated by the spinal accessory or cranial XI nerve.
Stand behind you patient. Place your stabilizing hand over the
patientís posterocentral area of the thorax. Place your resisting hand
over the posterior occipital area.
Tell the patient to extend his/her neck slowly while you gradually
increase the resistance until you determine patient overcome resistance.
LATERAL FLEXION
Lateral flexion of the cervical spine is primarily accomplished by
the Scalenus anticus, Medius, and posticus, which have innervation,
derived form the anterior primary divisions of the lower cervical
nerves.
Stand to the side of the patient. Place your stabilizing hand on
the right shoulder to prevent substitution of shoulder elevation. Then
place the open palm of your resisting hand on the right side of the
patientís head.
Ask the patient to laterally flex his head, while you gradually increase
resistance until you determine the maximum patient overcome resistance.
ROTATION-LATERAL FLEXION
The contralateral sternocleidomastoidius muscle innervated by the
signal accessory, XI cranial nerve, primarily accomplishes global
rotation of the cervical spine.
Stand in front of the patient. Place your stabilizing hand on his
right shoulder to test the muscle for left global rotation. Place your
resisting hand along the left side of the patientsí mandible.
Ask the patient to rotate his head slowly, while you are gradually
increase your pressure to determine maximal patient overcome resistance
power. Always check bilaterally for al applicable tests.
Whenever your examining the cervical spine with a Kinesiological
examination it is mandatory to run the test you learned for the upper
extremities to determine any pathology which may refer symptoms into the
extremities including cord tumor, disc prolapse, stenosis, and brachial
plexus pathologies.
TEMPOROMANDIBULAR JOINT TESTING
OPENING THE MOUTH
The external pterygoid muscle primarily accomplishes opening the
mouth with innervation derived by both the Trigeminal nerve-mandibular
division, and the pterygoid branch.
Place your open palm of your resisting hand beneath the patientís
jaw, and instruct him to open hi mouth, while you are gradually increase
the pressure of resistance. Determine the maximal patient overcome
resistance power. The patient should normally be able to over
maximal resistance (patient should be able to open his mouth 3 finger
girths) power.
CLOSING THE MOUTH
The Masseter muscle innervated by the Trigeminal nerve and
Temporalis muscle innervated by the Trigeminal nerve primarily
accomplishes closing the mouth.
EXAMINATION OF THE SHOULDER
FLEXION
Flexion of the shoulder involves primarily the anterior portion of
the deltoid and the Coracobrachialis muscles. The deltoid is innervated
by the Axillary nerve-C5 and the musculocutaneous nerve, C5-C6,
innervates the Coracobrachialis. In order to evaluate this nerve level
the following muscle testing procedure is recommended.
When testing the patientís right shoulder stand behind the patient
with your left hand upon their right Acromion. This hand will be
utilized for stabilization of the scapula and will palpate the anterior
deltoid region while testing. Grasp the biceps region of the left arm
proximal to the elbow. Bring the patientís elbow flexed to 90 degrees,
and tell them to begin flexion of the shoulder. As the patient begins
flexion, increase your resistance carefully to determine the maximal
resistance the patient can overcome. Always test both shoulders to
provide a bilateral comparison, and register your data accordingly.
EXTENSION
Extension of the shoulder involves primarily the Latissimus dorsi,
Teres major and posterior portion of the deltoid. The Thoracodorsal
nerve, C6, C7, C8, innervates the Latissimus dorsi; the Teres Major by
the lower subscapular nerve, C5 and C6; and the Posterior portion of the
deltoid innervated by the Axillary nerve, C5, C6.
Maintain the same position as for the flexion examination except
that you move your right thenar eminence and palm over the posterior
portion of the humorous. Always try to palpate with the stabilization
thumb for muscular tone; in this case posterior deltoid region. Try to
palpate the triceps with the resistance thumb.
Simply have the patient flex his elbow and slowly extend his arm
posteriorly. As the patient moves his shoulder into extension,
increase pressure as you did in flexion testing, until you determine the
maximum amount of resistance that he can overcome.
ABDUCTION:
Abduction of the shoulder involves primarily the mid portion of the
deltoid and the Supraspinatous musculature. The mid deltoid is
innervated by the Axillary nerve, C5, C6 and the Supraspinatous is
innervated by the Suprascapular never C5, C6.
Slightly adjust your position to the patient. This will allow your
stabilization hand to glide slightly lateral so you can palpate the mid
portion with the deltoid. Also, move your resistance hand slightly
lateral so your palm contacts the lateral Epicondyle area.
Have the patient abduct his arm gradually as you increase
resistance pressure until you determine the maximum resistance the
patient can overcome.
ADDUCTION
Adduction of the shoulder involves primarily the Pectoralis major
and the Latissimus dorsi musculature. The Pectoralis major is
innervated by the medial and lateral anterior thoracic nerve, C5, C6,
C7, C8, T1 and the Latissimus dorsi is innervated by the Thoracodorsal
nerve, C6, C7, and C8.
Move your stabilization hand anteroinferiorly upon the Acromion so
that palpation of the Pectoralis major will be possible.
Have your patient adduct his arm while your gradually increase the
degree of resistance, until determination of maximal resistance that the
patient can overcome is made. Record you data.
EXTERNAL ROTATION
External Rotation of the shoulder involves primarily the Infraspinatous
muscle innervated by the Suprascapular nerve, C5 and C6 and the Teres
minor muscle innervated by a branch of the Axillary nerve. C5.
Stand directly lateral to the patient and have the patient bend his
elbow to 90 degrees. Stabilize his/her flexed elbow against his waist
with his forearm in a neutral position. Grasp his wrist with your right
resistance hand.
Ask your patient to move his arm in a rotational manner outward
while you gradually increase the resistance until determination of
maximal resistance the patient can overcome is recorded.
INTERNAL ROTATION
Internal Rotation of the shoulder involves primarily the following
musculature and corresponding innervation.
1.
Pectoralis Major Innervated by the medial and
lateral anterior cervicothoracic nerves C5, C6, C7, C8, and T1.
2.
Latissimus Dorsi innervated by the
Thoracodorsal nerve, C6, C7 and C8
3.
Subscapular innervation by the upper and lower
subscapular nerves, C5 and C6
4.
Teres major innervated by the lower
subscapular nerve C5 and C6.
The stabilization hand and your body position remain the same.
Move your resistance hand so that your fingers wrap around the wrist and
the palm over the radial styloid process.
Ask your patient to gradually move (rotate) their arm in front of
their body while you carefully increase resistance against his wrist.
Note the maximal resistance factor.
SCAPULAR ELEVATION
Scapular Elevation of the shoulder involves primarily the Trapezius
innervated by the spinal accessory nerve, also know as the XI cranial
nerve; and the Levator Scapulae innervated by branches of C4 and C4 and
in many cases branches from the dorsal scapular nerve, C5.
Move behind you patient and place your hands directly upon each
Acromion. Make sure that you have your thumb posteriorly placed over
the trapezius muscle for palpation during the test.
Ask the patient to shrug their shoulder, and gradually increase downward
pressure through your resistance hands. Note any difference in the
elevation of the two sides. Scapular elevators normally overcome your
resistance. Records your data.
SCAPULAR PROTRACTION
Scapular Protraction of the shoulder involves primarily the Serratus
anterior muscle innervated by the Long Thoracic Nerve, C5, C6, and C7.
Scapular protraction refers to the motion of the scapula during the last
few degrees of reaching. Here scapula moves Anteriorly on the thorax.
Remain standing posterolaterally to the patient. Have the patient
flex their arm 90 degrees remaining parallel to the floor. Cup his
elbow with your resistance hand sliding your stabilizing hand over the
patientís spine preventing substitution or recruitment of the trunk
rotation for the shoulder protraction.
Ask the patient to move his bent arm forward as if he were reaching
forward with his elbow and gradually increase your resistance to this
anterior reaching motion, until the maximum resistance they can overcome
occurs. During the testing of shoulder protraction, always note the
motion of the scapulae for any winging which indicates weakness of the
Serratus anterior muscle. This may also be noted by observing the
patient do push-ups or pushes against a door. Record your data.
SCAPULAR RETRACTION
Scapular retraction of the shoulder involves primarily the Rhomboid
major innervated by the dorsal scapular nerve C5 and the Rhomboid minor
innervated by the dorsal scapular nerve, C5.
Now move to the front and face the patients. Place your palms just
anterior to the Acromion and the fingers reaching around the lateral
aspect of the shoulder over the medial deltoid and behind the
shoulders. Have the patient throw him or herself into a position of
attention (as in the military). Now slowly apply force with your
fingers trying to bend the shoulders forward around your thumbs without
digging your fingers into their musculature.
KINESIOLOGICAL TESTING OF THE ELBOW
FLEXION
Flexion of the elbow involves primarily the Brachialis innervated by the
musculocutaneous nerve, C5, C6 and the Biceps when the forearm is
supinated innervated by the musculocutaneous nerve, C5, C6.
Remain standing in the front of the patient after scapular
retraction testing. Grasp the patientís right arm just proximal to the
joint with your left stabilizing hand. Grasp the patientís right
forearmís palmar surface just proximal to the carpal bones.
Ask the patient to flex his arm slowly. When his arm flexion
approaches 45 degrees, begin to increase resistance until the maximum
resistance the patient can overcome is noted. Always test bilaterally
and record the date.
EXTENSION
Extension of the elbow involves primarily the Triceps innervated by
the radial nerve.
Remain the same initial position for testing flexion. Have the
patient extend their arm slowly from the flexed position. Before
reaching a position of approximately 90 degrees, gradually increase
resistance to determine overcome resistance power.
SUPINATION
Supination of the elbow involves primarily the Biceps innervated by
the musculocutaneous nerve, C5 and C6 and the Supinator muscle
innervated by the radial nerve, C6.
With your left hand, grasp the patientís right forearm with your
thenar eminence on the head of their radius while rapping your fingers
around the posterior aspect of the ulna.
Have the patient initiate forearm Supination from a Pronation
position. Ask them to begin Supination as you gradually increase your
distance until you determine patient overcome resistance and record you
findings.
PRONATION
Pronation of the elbow involves primarily the Pronator Teres muscle
innervated by the median nerve, C6 and the Pronator Quadratus muscle
innervated by the anterior interosseous branch of the median nerve, C8
and T1.
Grasp the patientís forearm with your right hand opposite the
position you maintained for testing Supination with your thenar eminence
against his volar surface.
Have the patient initiate forearm Pronation from a Supination
posture. Ask them to begin Pronation as you gradually increase your
resistance until you determine patient overcome resistance force and
note degree.
KINESIOLOGICAL TESTING OF THE WRIST AND
HAND
WRIST
Wrist extension Ė C6
The following group of muscles primarily accomplishes extension of the
wrist.
1.
Extensor Carpi radialis Brevis innervated by
the radial nerve C6 and perhaps some C7.
2.
Extensor Carpi radialis longus innervated by
the radial nerve C6 and perhaps some C7.
3.
Extensor Carpi ulnaris innervated by the
radial nerve, C7.
Place your left stabilizing hand upon the wrist of the patientís
right wrist rapping your fingers under their volar aspect of the wrist.
Ask the patient to extend his wrist fully. Place the palmar aspect of
your right hand over his fist, exert force, and try to take his wrist
out of the extended position. Normal power data would correlate with an
inability to move the patientís wrist out of its position.
WRIST FLEXION C7
The primary flexors of the wrist are the flexor Carpi radialis muscle
innervated by the median nerve, C7 and the flexor Carpi ulnaris muscle
innervated by the ulnar nerve, C8 and perhaps some T1.
Keep your stabilization hand in the same position as extension
testing. Ask the patient to flex their wrist fully while maintaining a
closed fist. Place your resistance hand over their fist, ask the
patient to resist and attempt to translate the wrist out of flexion.
Wrist Supination and Pronation were demonstrated in the elbow section
above.
FINGER TESTING
FINGER
EXTENSION Ė C7
The following group of muscles primarily accomplishes extension of
the fingers.
1.
Extensor Digitorum Communis innervated by the
radial nerve, C7
2.
Extensor Indicis muscle innervated by the
radial nerve, C7
3.
Extensor Digiti Minimi muscle innervated by
the radial nerve C7
Have the patient extend their metacarpophalangeal joints, while
leaving their proximal interphalangeal joints in flexion. Slide your
stabilizing hand so that your thumb grasps the radial base wrapping your
fingers around the volar surface of the wrist. Place your resistance
hand over the dorsal aspect of the fingers. Attempt top force the
phalanges into extension while the patient resists.
FINGER FLEXION Ė C8
The following group of muscles primarily accomplishes flexion of the
fingers.
1.
Flexor Digitorum profundus muscle innervated
by the ulnar nerve, C8 and T1 with further innervation from the anterior
branch of the median nerve (Distal Interphalangeal Joints).
2.
Flexor Digitorum Superficialis muscle
innervate by the median nerve C7, C8 and T1 (Proximal Interphalangeal
Joint).
3.
Lumbricals are flexors of the
metacarpophalangeal joint divided into medial two Lumbricals innervated
by the ulnar nerve, C8 and the Lateral two Lumbricals innervated by the
e median nerve, C7.
Ask the patient to flex his fingers into a loose fist. Then flex and
interlock your left hand into his right hand while still maintaining the
stabilization hand. Attempt to pull his fingers out of flexion. Note
any joints, which failed to maintain finger flexion. Normal study would
find all the joints remaining in flexion.
FINGER ADDUCTION Ė T1
Finger Adduction is primarily accomplished with the palmar Interossei
muscles innervated by the ulnar nerve C8 and T1 levels.
Ask the patient to keep their extended fingers together while you
attempt to pull the apart. Generally, most knowledgeable kinesiologists
test the fingers in pairs. Begin with the index and middle, followed by
the middle and ring fingers, and last the right and little fingers.
ABDUCTION Ė T1
Abduction of the fingers if primarily accomplished by the dorsal
Interossei muscles innervated by the C8 and T1 and the Abductor Digiti
Minimi muscles innervated by the ulnar nerve C8 and T1.
Ask the patient to abduct his extended fingers or spread hi fingers
and hold. The physician tryís to force his fingers together.
THUMB TESTING
EXTENSION
Extension of the thumb is primarily accomplished in the following
manner:
The Extensor pollicis Brevis extends over the metacarpophalangeal joint
and is innervated by the radial nerve, C7, the Extensor Pollicis Longus
Muscle extends the interphalangeal joint innervated by the radial nerve,
C7.
Ask the patient to extend his thumb. Attempt to push the thumb
into flexion. Check for weakness and correlated with the thumb
abductors which can cause thumb extension.
FLEXION
The Flexor Pollicis Brevis with its dual innervation of medial portion
by the ulnar nerve, C8 and the lateral portion by the median nerve, C6
and C7 act as flexors of the metacarpophalangeal joint. The Flexor
Pollicis Longus innervated by the median nerve, C8 and T1 would flex the
metacarpophalangeal joint.
Ask the patient to touch his hypothenar eminence with his thumb.
Grasp your thumb around the patients fully flexed thumb and attempt to
pull his thumb out of flexion. Note power and correlate bilaterally.
ABDUCTION
Abduction of the thumb is primarily accomplished by the Abductor
Pollicis Longus innervated by the radial nerve, C7 and the Abductor
Pollicis Muscle innervated by the median nerve, C6 and C7.
Maintain your stabilizing hand by placing your thumb over his
Pisiform and rapping your finger around his wrist. Ask the patient to
abduct his thumb completely, while your attempt to push the thumb back
into the palm. Correlate with thumb extensor, which can be secondarily
substituted to accomplish thumb abduction.
ADDUCTION
Adduction of the thumb is primarily accomplished by the Adductor
Pollicis (Oblique and Transverses) innervated by the ulnar nerve, C8.
Maintain your stabilization hand as you did in the abduction test.
While you hold the patientís thumb, ask the patient to adduct it, and
gradually increase resistance to determine patient overcome resistance
pressure.
PINCH MECHANISM OF THE THUMB AND INDEX
FINGER
The pinch mechanism demonstrates the integrity of long flexors and
extensors, which stabilize the interphalangeal, metacarpophalangeal, and
carpometacarpal joints. The Interossei and Lumbrical muscles must be
intact to assist this mechanism.
Ask the patient to touch his thumb and index finger together. Hook
your index finger at the junction of the two fingers and attempt to pull
them apart. A normal study would find that you would not be able to
pull the fingers apart.
THUMB AND LITTLE FINGER OPPOSITION
The Opponens Pollicis muscle innervated by the median nerve primarily
accomplishes this motion, C6 and C7 and the Opponens Digiti Minimi
innervated by the ulnar nerve, C8.
Ask the patient to touch the tips of his thumb and little finger
together. Grasp the patientís thenar eminence with one hand and his
hypothenar eminence with your other, and try to pull his thumb and
little finger apart.
EXAMINATION OF THE HIP AND PELVIS
PRIMARY MOVERS
As with the previous test, coordinate the motion integrity with motor
power and nerve level.
HIP FLEXION
The Iliopsoas muscle innervated by L2, 3 and 3, primarily accomplishes
flexion of the hip and pelvis.
Have the patient sit on the edge of the examining table. The
stabilization hand is placed over the iliac crest. Have the patient
raise their thigh from the table. Place your resistance hand upon the
distal end of the thigh and have the patient raise their thigh further
while you exert pressure. Determine the MOR (maximum overcome
resistance) and record your data. Repeat the test upon the other
thigh.
EXTENSION
Extension of the hip and pelvis is primarily accomplished by the
Gluteus Maximus innervated by the inferior Gluteal Nerve, S1.
Have the patient lie prone on the exam table and have the patient
flex their knee to relax the hamstring muscle. Place your forearm upon
the iliac crests resting your hand upon the gluteus Maximus and palpate
as you test the muscle. Place our resistance hand over the posterior
thigh region. Have the patient raise their thigh from the table while
you exert pressure down on the posterior thigh region just above the
knee. Record the patients MOR and test the opposite hip.
ABDUCTION
Abduction of the hip is primarily accomplished by the Gluteus
Medius innervated by the Superior Gluteal nerve, L5.
Have the patient lie on their side. Place your stabilizing hand
upon the patientís iliac crest. Ask the patient to abduct their leg.
Place your resistance hand over the lateral aspect of the leg and while
the patient is resisting attempt to push the legs together. Repeat the
test upon the opposite hip and record data.
ADDUCTION
The Adductor Longus muscle innervated by the Obturator Nerve, L2,
and 3,4 primarily accomplishes adduction of the hip.
Have the patient lie supine upon the table. Ask the patient to
abduct their legs while you exert pressure on the medial aspects of both
legs grasping them just above the ankles. Record your data.
KINESIOLOGICAL EXAMINATION OF THE KNEE
EXTENSION
Extension of the knee is primarily accomplished by the Quadriceps muscle
innervated by the Femoral nerve, L2, 3, and 4.
Have the patient sit near the edge of the table. Place your
stabilizing hand just above the patientís knee. Ask the patient to
fully extend their knee. With the knee fully extended, exert pressure
just above the ankle joint. Record data and test the other knee.
FLEXION
The HamstrIngs muscles primarily accomplish flexion of the knee.
1.
Semimembranosus innvrvated by the Tibial
portion of the sciatic nerve L5.
2.
Semitendinosus innervated by the Tibial
portion of the sciatic nerve L5.
3.
Biceps Femoris muscle innervated by the Tibial
portion of the sciatic nerve S1.
Have the patient lie prone on the exam table. Pace your stabilizing
hand over the thigh just above the knee. Ask the patient to flex their
knee while you resist this motion by containing just above the ankle
joint and exerting pressure. T specifically test the biceps Femoris
muscle externally rotate the patientís leg and test. To test the
Semimembranosus and Semitendinosus muscles more specifically internally
rotate the leg and test. Record data and test the opposite extremity.
Internal and External Rotation will not be tested as isolating the
specific muscle which would cause these motions cannot be accomplished
specifically. It must be noted however that their muscle power has been
tested during the flexion and extension tests.
KINESIOLOGICAL TESTING FOR THE FOOT AND ANKLE
The Kinesiological examination for the foot and ankle is divided
into testing Dorsiflexion and plantar flexion. Some of the muscles,
which cause these motions, also cause inversion and Eversion. The
tendons in front of the malleoli primarily cause Dorsiflexion of the
foot and this behind the malleoli yield plantar flexion.
The following muscles primarily accomplish Dorsiflexion of the foot.
1.
Tibialis Anterior innervated by the deep
Peroneal never L4 (L5)
2.
Extensor Hallucis Longus innervated by the
deep Peroneal nerve, L5.
3.
Extensor Digitorum Longus innervated by the
deep Peroneal nerve, L5.
It must be noted that any Pathomechanics, which prevent proper
nerve function, will result in foot drop and this nerve level can be
coordinated by the following examinations.
TIBIALIS ANTERIOR
Have the patient sit on the edge of the examination table. Grasp the
patientís lower leg with your stabilizing hand. Wrap you resistance
hand about the dorsum of the foot with your fingers under the foot. Ask
the patient to dorsiflex and invert his foot. Try to plantar flex and
evert his foot and record data. Test the opposite foot.
EXTENSOR HALLUCIS LONGUS
Have the patient sit on the edge of the table. Grasp the patientís
Calcaneus and stabilize the foot. Grasp the big toe with your thumb
over the nail area with your fingers under the foot. Ask the patient to
dorsiflex their toe and you offer resistance and attempt to push the toe
down. Be sure your resistance contact is distal to the interphalangeal
joint. If your contact is across the interphalangeal joint, you may
also be testing the Extensor Hallucis Brevis.
EXTENSOR DIGITORUM LONGUS
Have the patient sit on the edge of the table. The stabilization hand
is again upon the Calcaneus. Have the patient extend their toes. Place
your thumb across the toes and attempt to plantar flex the patientís
toes. Record our data and test the other foot. A normal study would
present unyielding toes.
PLANTAR FLEXION
The following muscles primarily accomplish plantar Flexion of the foot:
1.
Peroneus Longus and Brevis innervated by the
superficial Peroneal nerve, S1.
2.
Gastrocnemius and Soleus innervated by he
Tibial nerve, S1, S2.
3.
Tibialis Posterior innervated by the Tibial
nerve, L5.
4.
Flexor Digitorum Longus innervated by the
Tibial nerve, L5.
5.
Flexor Hallucis Longus innervated by the
Tibial nerve, L5.
PERONEUS LONGUS AND BREVIS
Ask the patient to sit upon the edge of the table. Stabilize the
Calcaneus with one hand. Place your resistance hand so that your thumb
rests against the fifth metatarsal head. Have the patient plantar flex
and evert their foot while you oppose plantar flexion and Eversion.
Record data and test the opposite foot.
GASTROCNEMIUS AND SOLEUS
Ask the patient to lie in the supine position. Grasp the patientís foot
and place it in the neutral position. Ask the patient to plantar flex
his foot while you offer resistance. Record the data (This primarily
records Soleus data).
FLEXOR HALLUCIS
LONGUS
Ask the patient to sit on the edge of the table. Again, stabilize the
Calcaneus. Instruct the patient to bend his great toe, while you resist
the plantar flexion. Perform the test on the opposite foot and compare
relative power.
TIBIALIS POSTERIOR
Ask the patient to sit on the edge of the table while you stabilize the
Calcaneus. Have the patient plantar flex his foot and invert his foot
while your offer resistance. Record the data and compare bilaterally.
Also, compare muscle power with other regional muscles, as they should
be in balance.
EXAMINATION OF THE LUMBAR SPINE
The Kinesiological examination of the Lumbar spine would include testing
the musculature associated with a nerve level in question. Thus the
tests you learned in the hip, pelvis and lower extremities would be
utilized to determine nerve level integrity. When ever you examine the
cervical spine or lumbar spine you coordinate the Kinesiological testing
you have performed with the nerve level. At the same time you test for
sensation
by
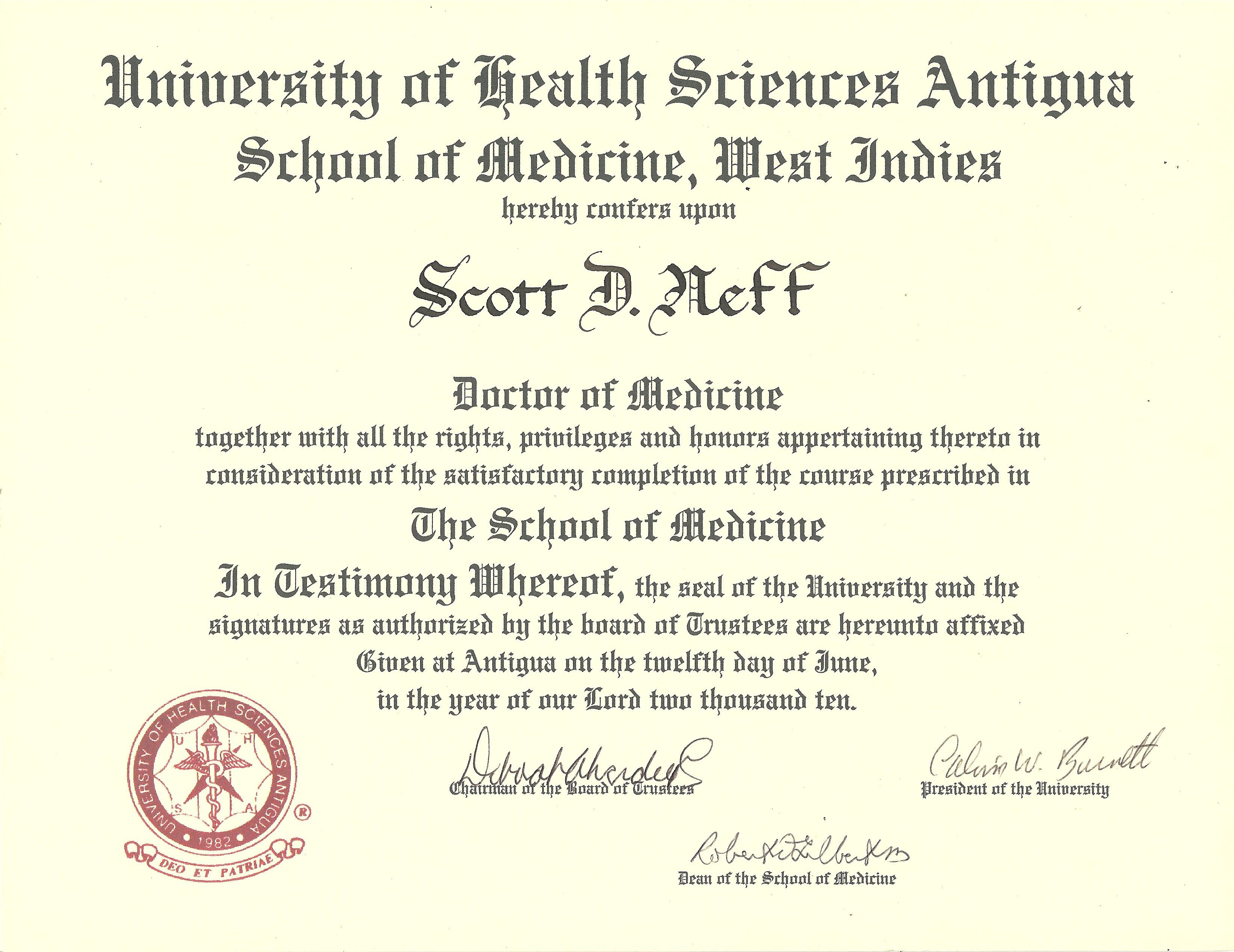
Scott D. Neff, DC DABCO CFE
DABFE FFABS FFAAJTS, 2010 Graduate Antigua School of Medicine, West
Indies created for the medical students of our world as well as a dedication to the
people of America and our world.
©
 "Why does this magnificent applied
science which saves work and makes life
easier, bring us little happiness? The simple answer runs, because we
have not yet learned to make sensible use of it." Albert Einstein 1931
|
![]()