
 |
Gram
Positive Organisms
I.
Gram Positive Cocci
Positive Catalase
Negative Catalase
1.
Staphylococcus
2.
Micrococcus Streptococcus
Peptostrepto/Enterococcus
Facultative Anaerobe Strict
Aerobe
Pyogenic Pneumo-coccus
Viridans/others
|
Staphylococcus
1. S.
aureus
+ Coagulase
+ Mannitol salt
Scaled skin
synd.
Toxic Shock
synd.
Food
poisoning
Dx: Disc
sensitivity
2. S.
epidermis
- Coagulase
- Mannitol salt
agar
Nocosomial
prosthetic infection
3. S.
saprophyticus
- Coagulase
- Mannitol salt
agar
UTI
|
Micro-coccus
NF skin
Free living
Non-parasitic
Micro-coccus,
Tetra-coccus,
Sarcinae
|
1. Group
A
b -
hemolytic
S.
pyogenes
NF skin
Pharyngitis
Cellulitis,
AGN
Rheumatic
fever
Scarlet
fever
2. Group
B
S.
agalactiae
Neonatal
sepsis
Meningitis
3. Non
A&B
S.
bovis
R/T Colon CA |
S.
pneumonia
Lancet shaped
Diplococcus (in
host; strepto-coccus in medium)
a -
hemolytic
+ Bile soluble
+ Quellung
reaction
Predisposing factor: Etoh, DM, renal dz, AIDS
False +
serology d/t similar Ab w/ Klebsiella and H.pneumo. |
1.
Viridans
a -
hemolytic
- Bile soluble
S.
mutans
Dental
caries,
Most common
endocarditis post dental surgery
2. Others
a.
Non-hemolytic
b. Micro –aerophilic
Never
pathogenic |
1.
Pepto - streptococcus
Anaerobic
Normal
colony in mouth, colon
2.
Entero-coccus
Group D
Halophilic
b -
hemolytic
Grow on bile
E.
faecalis
Nocosomial
UTI
|
II. Gram Positive Rods
Spore & Exotoxin Producing
Non-Spore Producing
|
Aerobic |
Anaerobic |
Filamentous |
Non-filamentous |
Bacillus
1. B.
anthracis
**
Bamboo rods
Medusa colony;
Elliptical central spore; Saprophyte; Capsule;
Exotoxin ->
Anthrax - 3 forms: Cutaneous, GI, Respiratory (Woolsorter’s
dz)
2. B.
Cereus
Motile; No
capsule
Food
poisoning d/t toxins - sx after 12 hrs |
Clostridium
1. C.
perfringens
Capsule;
Food poisoning - 8 to 24 hrs after consumption of stews and
gravies. Gas gangrene
2. C.
tetani
** Tennis racket
w/ terminal spores; Motile; Tetanus
Lockjaw, muscle
spasm
3. C.
botulinum
Subterminal
spore, Contaminated canned food -> paralysis; Infant (honey).
Neurotoxin- destroyed by heat, virus
induced
4. C.
difficile
Abx assoc.
pseudo-membranous colitis |
1.
Actinomyces israelii
Microaerophilic/ Obligate anaerobe
NL oral
cavity
Invade
tissue post trauma eg. Tooth extraction
Sulfur
granules
2.
Nocardia asteroides
Strict
Aerobic
Acid fast
Pulmonary
infection from soil |
1.
Corynebacterium diphtheriae
+ Tellurite agar,
+ Catalase; Twisted rods;
+ Exotoxin due to lysogenic bacteriophage; Diphtheria
Sx:
** pseudomembranous pharynx, Bullneck
2.
Listeria monocytogenes
b-hemolytic,
+ Catalase
Motile,
pseudopod; In unpasteurized milk; Listeriosis - Grow in
non-immune macrophage
3.
Erysipelothrix
In decaying
matter; Causes erysipeloid (erythematous skin); Traumatic
inoculation esp. in butcher/fisherman |
Gram Negative Organisms
|
Cocci |
Rods |
No Cell Wall |
|
Neisseria -
Diplococci
+
Capsule and Fimbriae
+ Oxidase;
Fastidius (Grows with CO2 and blood); Facult anaerobe
1.
N. meningitidis
IgA
protease; Get into bld stream and enter meninges. Nasal
carriers. Fimbriae.
Dx:
Spinal tap, CO2 enriched BAP
2.
N. gonorrhea
Chocolate agar w/ CO2
Dx: Male
– 2-7 days purulent urethral d/c with dysuria. Female- asx
(smaller urethra).
Enzyme- sugar
ferment.
Thayer-Martin
agar (has Abx).
Medicolegal. Other
Neisseria (not grow on T-M agar).
|
1.
Strict Aerobic
Pseudomona aeruginosa
Motile
**
Water soluble greenish
pigment
Common
in burns, cystic fibrosis
2.
Strict Anaerobic
Bacteroides
3.
Others
(See
below) |
1. Mycoplasma
- Urease;
No cell wall (Gm – d/t CM); Smallest cell; Pleomorphic
Sterol in CM. Older name =
PPLO.
M. pneumoniae
Fried egg colonies
Mycoplasma agar
Serology – Fluorescent Ab
M. hominis
Post abortion and post partum
infection; from own genital NF
2. Ureaplasma
No cell wall (Gm – d/t CM)
Smallest cell; Sterol in CM;
+ Urease;
Non-gon,non-chlam
urethritis |
Others
- Straight
Others - Curved
Respiratory
|
Zoonotic
|
Enterobacteriacea
|
Curved
|
|
1.
Haemophilus
H.
influenzae
Coccobacillus
Complex lab media of hematin (Factor X) and NAD (Factor V)
Resp.
transmission
[[H. ducreyi
(Chancre)
Painful,
soft, ulcerating chancroid; Buboes, Satellite lesions
H.
aegyptius
Conjunctivitis]]
2.
Bordetella pertussis
Coccobacilli, + Fimbriae (Not virulent w/o it)
Droplet
infxn;
Whooping
cough; Stages: Catarrhal, non-productive paroxysmal cough,
convalescence
3.
Legionella pneumophilia
+ Silver
impregnation stain (Gm
St not good)
Fastidius (Requires L-cysteine and FE3+)
Colonies
“ground grass”
Parasite
of protozoa
Necrotizing multifocal PNA, multiplies w/in monocyte-macrophage
Fluorescent Ab
Test |
1.
Yersinia pestis
Gm -
bipolar
Bubonic plague
vector =
flea
Fever,
buboes – up to 70% mortality w/o tx
Primary
PNA = plague
Do Gram
stain of buboe
2.
Brucella
Undulant fever
(24hr nl
then fever then normal; peaks in the evening)
Enriched
medium
B.
abortus = cow
B.
melitensis =
goat
Transmitted by unpasteurized milk
Dx: Serology
3.
Francisella tularensis
Coccobacillus
Bite of
vector (tick or deer fly)
Tularemia
**
Infects reticular endothelial
organs
Buboes
4.
Pasteurella multocida
Coccobacillus
Cellulitis due to cat/dog scratch/bite
Dx:
Culture on BAP |
All
ferment glucose, reduce nitrate, Oxidase negative
1.
Escherichia coli
EMB agar;
Most common cause of
UTI
2.
Shigella
S.
Sonnei -
Shigellosis; Dysentery;
3.
Salmonella typhi
Stool
- EMB and deoxycholate; + H2S
Typhoid
fever; Salmonellosis x typhoid. In chicken containing food.
4.
Yersinia pestis
Bipolar
staining (more concentrated at the ends).
Plague,
Vector = flea (bite)
5.
Serratia
Inducible enzyme. Opportunist.
6.
Citrobacter
Citrate
as sole source of nutrient. Opportunist.
7.
Klebsiella pneumoniae
Now just
respiratory infxn. Current jelly sputum.
8.
Enterobacter
Peritrichous flagella. Opportunist.
9.
Proteus, Providencia, Morganella
In AIDS
pt only |
1.
Vibrios cholerae
Polar
flagella
Halophilic
Fecal
contamination
**
Rice water stool
2.
Campylobacter
Polar
flagella
C.
jejuni and C. enteritis
Diarrhea
C.
fetus
Abortion in animal, Sepsis in human
3.
Helicobacter pylori
Peptic
ulcer and gastritis
+ Urease-
NH4 OH act as buffer
|
III. Non Gram Staining Organisms
A. Spirochetes
Axial rod through spiral - (spirillum
w/o axial rod) Dx: Dark Field or E.M.
|
Treponema |
Borrelia |
Leptospirosis |
|
1.
Treponema pallidum
(Syphillis)
2.
T. pertenue
( Yaws)
3.
T. carateum
(Pinta)
|
1.
Borrelia recurrentis
(Relapsing
fever)
2.Borrelia burgdorferi
(Lyme dz)
|
|
B. Acid fast
rods, Chlamydia, and Rickettsia
|
Acid Fast Rods |
Chlamydia |
Rickettsia |
|
A.
Mycobacterium
Aerobes
Slow
growing
Stain:
Carbolfuschins, acid alcohol, methylene blue
1.
M. tuberculosis
(Tuberculosis)
Droplet infection or unpasteurized milk
Focus of
infection – Lungs (Exotoxin) PPD skin test (protein ppt
derived test)
If +
test – do CXR and sputum cx
AIDS pt
– M. kansasii
and
M. avium
2.
M. leprae
(Leprosy)
Grow on
foot pads of mice and armadillos;
New
cases from prolonged contact with infected
Trans:
nasal mucosa, skin lesions, insects
Granulomatous dz of PNS and nasal mucosa. Brown rash becomes
necrotic, infects cartilage and bone.
Dx: Acid
fast stain
B.
Nocardia – see Gm Pos Rods |
Reproduce via endocytosis/ multiplication (elementary body®
reticular body)
1.
C. psittaci
(Psittacosis)
TWAR
strain – does not need bird vector
2.
C. pneumoniae
(Walking PNA)
Droplet
transmission, Nosocomial infection
3.
C. trachomatis
a.
Trachoma = Chronic conjunctivitis (Strain A,B,C)
Contact
or fomite
b.
Non-gonococcal urethritis
(Str D®K)
leading cause of STD, male – purulent d/c, dysuria,
med-legal
c.
Inclusion conjunctivitis
(Str D®K),
In newborns d/t mother w/ NGU
d.
Lymphogranuloma venerum (LGV)
(Str
L1-3) Buboes |
|
FUNGUS
I. DIMORPHIC
|
1. North American
Blastomycosis
(Gilcrist’s Disease)
(Blastomyces dermatitidis).
Suppurative and granulomatous
skin lesions esp. in skin, lungs, bones.
** One blastospore. 2
Types- 1). Cutaneous: skin- purulent, Lesions- elevated
edges. 2). Systemic: Resp tract- disseminated via blood to
tissues and bones.
2. South American
Blastomycosis
(Paracoccidioides)
(Blastomyces brasiliensis
or Paracoccidioides brasiliensis)
Chronic granulomatous disease of skin, mucous membrane, LN,
organs. Saprophyte. Require warm temp. POE= Mouth.
**Large LN. ** Many blastospores.
4 Types: Cutaneous (mucosal), Lymphatic, Visceral,
Mixed-type. |
3.
Coccidioidomycosis
(Valley Fever, San Joaqhin Fever).
(Coccidioides immitis)
Yeast-
spherule with endospore. Barrel-shaped arthrospore. Most
infectious of the system mycoses. Need blood. FOI=
Lungs. Pigeon feces. In Southwest.
4. Histoplasmosis
(Histoplasma capsulatum)
Spikelike tuberculate macroconidia. Pigeon feces, infected
bat guano. Central/Eastern US. Reticuloendothelial system.
Grow within macrophage.
3 Types:
1). Primary- lungs calcification in parenchyma. 2).
Progressive- Emaciation, leukopenia. 3). Disseminating-
Febrile and enlargement of reticulo-endothelial organ eg.
Spleen, liver.
Serological-
need titer 1:32 or higher. |
5.
Tinea Versicolor
(Malassezia
furfur)
Superficial skin.
*Hypo-pigmented areas. More frequent in hot humid
weather. Lesions contain both budding yeast cells and hyphae.
Obtained by trauma. Dx- KOH prep.
6.
Sporotrichosis
(Sporotrichum
schenckii)
Traumatic inoculation. Hyphae- 3 to 5 macroconidia in
clusters. Nodular lesion that forms indolent (hard) ulcers
(lymphatic pustule) in LN, skin, or subcutaneous tissues.
Saprophyte. Pyogenic infection spread along lymph system to
bones, eyes, CNS. |
II. NON – DIMORPHIC
|
Yeast Only |
Mold Only
|
|
Other |
|
1.
Cryptococcosis
(Cryptococcus neoformans)
The
most common life-threatening fungal disease in AIDS pts.
Immuno-compromised. **Yeast with
large capsule. Bird feces with soil. Infects esp.
brain and meninges.
2. Candidiasis
(Candida albican)
NF.
Opportunist (esp. in DM- overgrowth d/t high sugar = thrush
in mouth). Moist skin. Yeast and
**pseudohyphae (chains of blastospores that do not
break off, look like hyphae). **Grows on
Corn meal agar (poor
nutrition for other fungus). 4 types: Mucous membrane=
Thrush, Cutaneous (vaginal, baby), Pulmonary, CNS. |
1.
Dermatomycosis
Grows on derma (skin, hair, nail).
The only communicable fungal infection. 3 Genera:
1). Microsporum (leaf shaped). 2). Trichophyton (macroconidia-
bat shaped). 3). Epidermophyton (Pingpong paddle shape).
Dermal infection (keratin).
Tinea = Tinea
pedis (feet), unguium (nail), cruris (jock-itch), corporis
(trunk), barbae (beard), capitis (ringworm on scalp),
imbricata (scales), favosa (honey-comb).
2.
Tinea Nigra (Cladosporium werneckii)
An
infection of the keratinized layers of the skin. Pleomorphic.
Brown to black macules on
palmar aspect of the hands (due to melanin-like pigment in
the hyphae).
3.
Maduromycosis
(Madura foot, Mycetoma)
**Clubbed shaped foot. (2X-3X normal size). Caused by
variety of filamentous fungi. Exogenous source, d/t trauma.
Occurs in the tropics and subtropics. Human pathogen that
reproduce sexually.
4.
Geotrichosis
(Geotrichum
species)
Infection is endogenous from mouth and intestine. Also
exogenous (soil). Immunocompromised pt. Geotrichum
candidum - seg-mentation of hyphae into
arthrospores
(brick-shaped).
5.
Aspergillus
(Aspergillus
species)
May
cause allergy. Opportunist. Inhaled spores. Separate hyphae.
Colonizing tuberculous cavity in lung. Cause PNA. |
6.
Mucormycosis (Mucor species)
Rapidly
fatal. Acute inflammation and vascular thrombosis. Cause=
hyphae invade walls and lumen of blood vessels.
**DM. Pulmonary
mucormycosis in DM- fatal (2-10days duration). Source= soil,
manure, fruit, bread mold. Ulcerative colitis in non-DM with
peritonitis, death.
7.
Rhizopus
Saprophytic. ** Esp in DM,
burns, leukemia. Airborne asexual spores.
Proliferates in walls of bld vessels esp. paranasal sinus,
lungs, gut. Cause necrosis distally. Nonseptate hyphae
broad, branches form right angles.
8.
Pseudallescheria
(Pseudallescheria
boydii).
Separated hyphae resemble Aspergillus.
** Conidia (pear-shaped) with
brownish-gray mycelium.
9.
Rhinosporidiosis
(Rhinosporidium seeberi)
Infect
mucous membrane of nose, eyes, ears, larynx, vagina, penis. Polyps. Cause=
Swimming in stagnant water.
Sx= painless itching with mucoid discharge. Develops into
tumors. Sporangiospore mold.
10. Chromoblastomyces or Verrucous dermatitis.
Caused
by a wide variety of fungi. Warty cutaneous nodules.
Infection by trauma. Simulates a patch of ringworm. |
1.
Actinomycosis
(Actinomyces
israelii)
Procaryotic Gram +. Chronic suppurative and granulomatous
lesions. **Sulfur granules
on skin. Anaerobic. Endogenous- NF of mouth. Enter
via trauma. Lumpy jaw. 3 Types: Cervicofacial, thoracic,
abdominal.
2.
Nocardiosis
(Nocardia
species)
**Strict
Aerobic.
Some acid fast.
Exogenous disease- soil. Suppurative and granulomatous
subcutaneous dz with swelling, abscess. 3 types: 1).
Mycetoma (unilateral infection of extremity), 2). Pulmonary
infection (N. asteroides). 3). Systemic
3.
Pneumocystis
(Pneumocystis
carinii)
PNA in
AIDS. Analysis of rRNA, mtDNA, enzyme= fungus. But not grow
on fungal media and antifungals are ineffective. But,
controlled by antiprotozoan. Has cystic forms and
sporozoites. Transmission by inhalation, but not invade lung
tissue. Cyst in alveoli cause frothy exudate that blocks gas
exchange. |
For the
Medical School and Chiropractic Students of
America by Scott D. Neff, DC DABCO MSOM MPS-BT DE IDE IME CFE DABFE FFABS FFAAJTS
2010 graduate Antigua School of Medicine, West Indies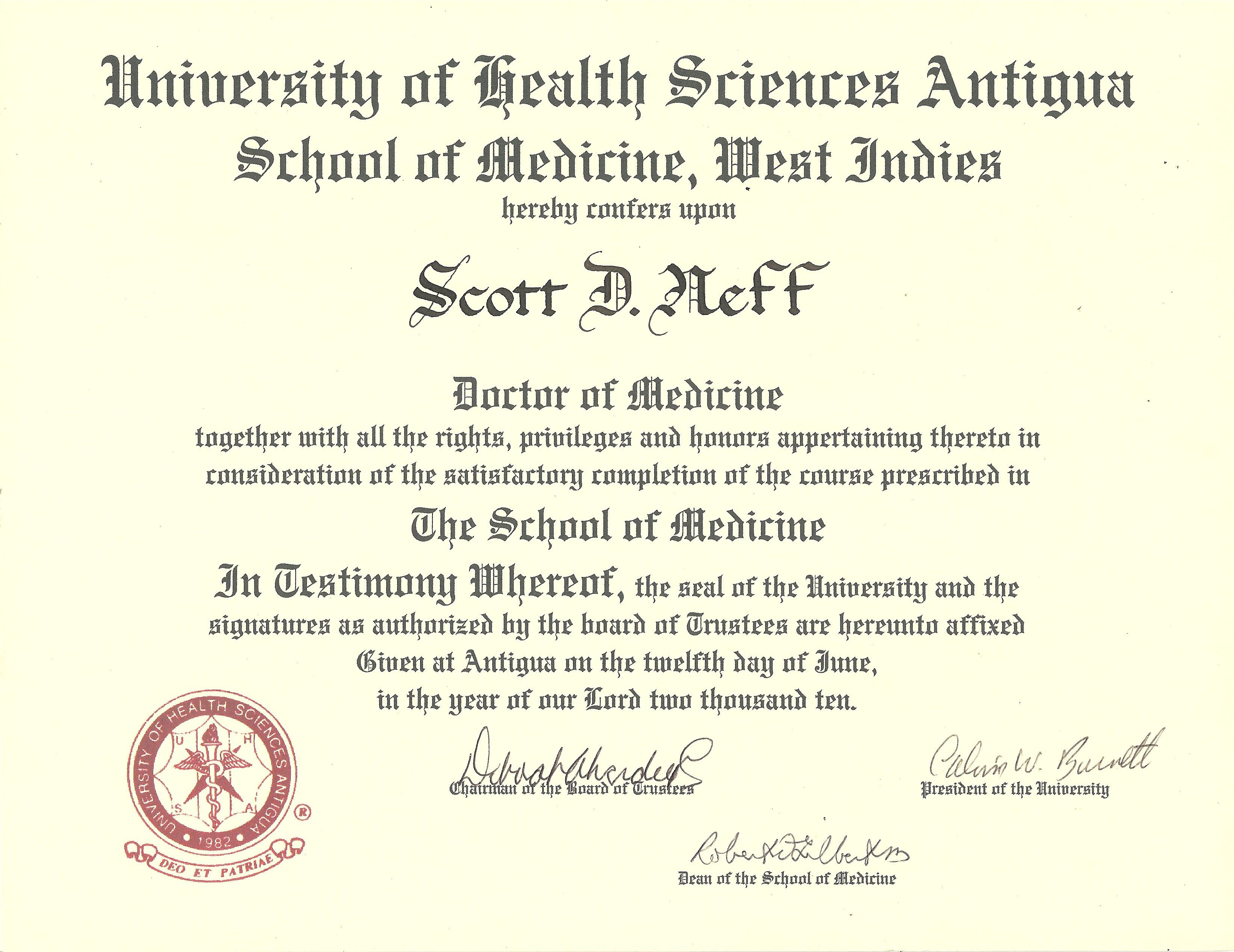
|
![]()